Blood
Sample Transportation in Laboratory Explained
Feb 25 2022
From pathology to vaccine development, sample transportation is one of the most important stages of the preanalytical pathway. While transporting samples from A to B may seem like a simple task, a variety of factors make the process challenging, complex and highly specialised. Ultimately, sample transportation can have a direct impact on results. This is why every laboratory should have clear guidelines in place to streamline sample transportation processes and safeguard specimens.
Want to know more about sample transportation in laboratory? Read on for our complete guide to sample transportation, covering everything you need to know about collection and storage protocols, temperatures, freeze drying, health and safety precautions and more.
Why is a good sample transportation strategy important?
A good sample transportation strategy is about more than simply moving specimens from one place to another. In laboratories, best-practice sample transportation works to achieve the following goals:
- Eliminating sample contamination
Transportation exposes laboratory samples to a variety of risks, including contamination. This can occur when samples are being transported between locations during transit or in the laboratory. For example, this can occur when a storage vessel is cracked and contaminants such as oxygen or bacteria particles contact the sample. For this reason, samples are often transported in Styrofoam boxes or insulating vacuum flasks. Incorrectly sealed containers, close proximity to other samples and exposure to airborne laboratory contaminants can also pose a risk.
- Avoiding delays in laboratory results
One of the main goals of a good sample transportation strategy is to minimise and ideally eliminate delays in laboratory results. Ideally, sample transportation should see specimens travel between destinations as quickly as possible, without any unplanned interruptions. In a worst-case scenario, a flawed sample transportation strategy could result in specimens being lost or destroyed.
- Preserving the integrity of samples
The moment samples are extracted from their source and stored in a vessel, their integrity is at risk. A good sample transportation strategy should take steps to preserve the integrity of samples during every stage of transport. This includes transport from the collection site to the laboratory, as well as transport within the laboratory.
Most laboratories require serum samples to be stored at temperatures of −20°C or less during longer periods of transport. During transit, they should be stored in portable fridges or on frozen ice packs. Other sensitive specimens, such as blood samples, may be damaged by agitation, exposure to daylight and other physical factors.
What are the rules for sample transportation?
Every laboratory has its own unique set of rules for sample transportation. Some are developed inhouse by laboratory managers and others are based on local, national and international sample transportation standards. Below, we take a closer look at some of the governing bodies and organisations that publish sample transportation in laboratory guidelines:
- International Organisation for Standardisation (ISO)
The International Organisation for Standardisation published guidelines for a myriad of fields and specialised areas, including transportation of scientific samples. For example, the ISO 15189:2012 “specifies requirements for quality and competence in medical laboratories” and is often used to design quality management systems and assess competence.
ISO/CD 20658 is even more specialised and designed exclusively for sample transportation in laboratory settings and in vitro diagnostic test systems. It’s still under development however when launched, it will outline “requirements for collection and transport of samples” by medical labs. It will build on the 20658:2017, which outlines gold-standard methods for the collection, transport, receipt and handling of clinical samples.
- Clinical Laboratory Standards Institute (CLSI)
The volunteer-driven Clinical Laboratory Standards Institute is another highly respected industry body. It’s guidelines for handling and processing blood specimens are used by pathology labs and health care centres in the United States.
- Clinical Laboratory Improvement Amendments (CLIA)
In the United States, clinical testing laboratories are strictly regulated by the government. This is an enormous responsibly, with roughly 200,000 clinical laboratories currently offering testing services in the USA. This includes hospital-based and physician office labs, as well as independent and privately-operated centres. Other laboratories also carry out testing, including public health clinics, community health centres, ambulatory surgery centres, nursing facilities, hospices, home health agencies, blood banks and more.
All labs performing in vitro diagnostic tests on humans must comply with rules published by the Clinical Laboratory Improvement Amendments (CLIA) and enforced by the Centers for Medicare and Medicaid Services (CMS).
The importance of labelling
Labelling has an important role to play throughout the sample transportation pathway. As soon as a sample is collected, whether it’s a geological sample extracted from a mine site or a serological sample for analyte analysis, it must be immediately labelled. This ensures the sample can be tracked and traced from the moment it leaves the collection site.
When samples reach the laboratory, they’re given a unique laboratory identification number. Generally, this should include information about the patient or the source where the sample was collected. Once again, this unique laboratory identification number allows lab technicians to track and trace the sample as it moves through analysis processes.
Transporting biological materials
When transporting biological materials, laboratories must meet an array of rules and regulations. In Europe, overland transport of dangerous goods is governed by the International Carriage of Dangerous Goods by Road (ADR) and Rail (RID). Samples transported by plane are subject to rules enforced by the International Air Transport Association Dangerous Goods Regulations.
Transportation protocols are often determined by the nature of samples. For example, the World Health Organisation (WHO) Surveillance Guidelines for Measles, Rubella and Congenital Rubella Syndrome includes a section dedicated to the collection, storage and transport of specimens relating to MMR. The guidelines cover important steps like sample labelling, storage temperatures and centrifuge processes.
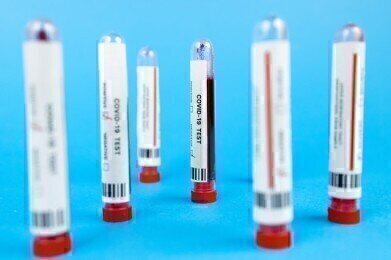
Transporting COVID-19 samples
The COVID-19 pandemic has underscored the importance of taking the right precautions when transporting clinical samples in the field and within the laboratory. The Centers for Disease Control (CDC) was quick to publish official Interim Guidelines for Clinical Specimens for COVID-19, including a special section on transporting samples. The guidelines are designed to maintain the biological integrity of samples and protect the health and safety of transport personnel and lab technicians.
To preserve the integrity of respiratory samples the CDC recommends storing specimens at temperatures of between 2°C and 8°C for up to 72 hours after collection. If delays are anticipated, the recommended storage temperature drops to -72°C or less.
The CDC has also published guidance for clinical laboratories handling, processing and transporting COVID-19 specimens. This includes handling all SARS-CoV-2 cultures according to Biosafety Level 3 (BSL-3) practices. All packing and transport procedures should comply with UN 3373 Biological Substance, Category B protocols.
How are blood samples transported?
Pathology plays a critical role in diagnosing disease and providing treatment. Pathology laboratories form the backbone of public and private health care systems, including the NHS. In the UK, the Royal College of Pathologists estimates around 95% of clinical pathways depend on pathology testing. Every year British pathologists conduct 500 million biochemistry and 130 million haematology tests. This equates to a huge 300,000 tests every business day.
Transportation of blood samples is fundamental to the pathology field. Moving samples between health centres, hospitals, pathology labs and testing clinics is an important stage in the preanalytical pathway and can directly influence results.
Below, we explore some key factors that must be considered when transporting blood samples:
- Analyte stability
Blood samples are particularly complex as they contain analytes that can lose stability over time. To maintain sample integrity, it’s important for pathology labs to adhere to fast turnaround times. It’s worth noting that transportation timeframes and conditions are usually determined by the target analytes. For example, some analytes are used to detect cancers and others are used as biomarkers for diseases such as diabetes or viruses like Hepatitis C.
The analytical methods being used to profile blood samples may also influence the required timeframes and transport conditions. Generally, most analytes remain stable for up to 12 hours with delayed centrifugation, excluding potassium, bicarbonate, LDH, osteocalcin, parathyroid hormone (PTH) and C-peptide. This timeframe can be increased to as long as 48 hours with immediate centrifugation and storage at 4°C.
- Physical influences
Physical and environmental influences, such as agitation or changes in temperature, can disrupt the preanalytical pathway and compromise the integrity of blood samples. This can occur both in the field and within the laboratory. For example, agitation during transport could create air bubbles in a blood sample, generate cellular debris or force blood cells to mix. All these scenarios instantly compromise the quality of the sample and jeopardise the reliability of results.
Managing sample transportation in laboratory workflows
With more than 300,000 biochemistry and haematology tests conducted every day in the UK, managing blood sample workflows is critical. Laboratories must ensure transportation logistics are well-established and uninterrupted. For example, a single blood sample must be able to travel seamlessly between a hospital ward or GP clinic and a pathology testing lab.
“Any delay from blood collection to centrifugation and analysis or any deviation from standard transportation conditions could potentially alter laboratory results and subsequently have a negative impact on patient safety,” reads a scientific article published in the journal, Diagnosis.
When the sample reaches the laboratory, transportation must also be streamlined. When transporting samples within the lab the process is either manual or automated. Both come with their own unique set of challenges, though automated transportation systems are generally preferred for their speed, accuracy and reliability.
Find out more about the highly specialised field of sample transportation from global laboratory relocation expert Andrew Powers in ‘Why a specialist approach is essential when it comes to moving samples’
Digital Edition
Lab Asia Dec 2025
December 2025
Chromatography Articles- Cutting-edge sample preparation tools help laboratories to stay ahead of the curveMass Spectrometry & Spectroscopy Articles- Unlocking the complexity of metabolomics: Pushi...
View all digital editions
Events
Jan 21 2026 Tokyo, Japan
Jan 28 2026 Tokyo, Japan
Jan 29 2026 New Delhi, India
Feb 07 2026 Boston, MA, USA
Asia Pharma Expo/Asia Lab Expo
Feb 12 2026 Dhaka, Bangladesh