Research news
Mitochondrial transfer offers a novel route to treat chronic nerve pain
Jan 09 2026
Researchers have reported that supplying healthy mitochondria to damaged nerve cells can reduce pain in models of diabetic neuropathy and chemotherapy-related nerve injury, pointing towards a strategy that targets the biological source of chronic pain
For millions of people who live with chronic nerve pain, even the lightest physical contact can be intolerable. Clinicians have long recognised that such pain often follows damage to peripheral nerves, yet effective long-lasting treatments have remained out of reach. A growing body of evidence suggests that an underlying problem lies in mitochondria failure – the energy-producing structures within cells – no longer functioning correctly in damaged neurons.
Recent research has now suggested a potential way forward by restoring mitochondrial health directly within damaged nerve cells. Using a combination of human tissue samples and mouse models, a team at Duke University School of Medicine, Durham, North Carolina, USA, has shown that the transfer of healthy mitochondria into compromised sensory neurons reduced pain associated with diabetic neuropathy and chemotherapy-induced nerve damage. In some experimental settings, the pain relief persisted for up to 48 hours.
Rather than masking pain signals, the approach aimed to correct what the researchers described as a fundamental cellular defect. By restoring the flow of energy that nerve cells require to survive and repair themselves, the intervention appeared to improve neuronal resilience and reduce inflammatory stress.
“By giving damaged nerves ‘fresh’ mitochondria – or helping them to generate more of their own – we can reduce inflammation and support healing,” said Dr. Ru-Rong Ji, director of the Centre for Translational Pain Medicine in the Department of Anaesthesiology at Duke University School of Medicine.
“This approach has the potential to ease pain in a completely novel way,” he added.
The findings built on the accumulating evidence that cells are able to exchange mitochondria, a phenomenon that researchers have increasingly viewed as a form of cellular support. Previous studies have suggested that mitochondrial transfer may influence a wide range of conditions, including obesity, cancer, stroke and chronic pain.
In this work, the team identified an unexpected role for satellite glial cells, which surround sensory neurons in peripheral nerve ganglia. These glial cells appeared to deliver mitochondria directly to neurons through microscopic structures known as tunnelling nanotubes. This mechanism had not previously been documented in the context of pain biology.
When this mitochondrial transfer was disrupted, nerve fibres began to degenerate, Ji explained, which led to pain, tingling and numbness. These symptoms typically emerged at the distal ends of nerves, such as those that supply the hands and feet, where energy demands are high.
“By sharing energy reserves, satellite glial cells may help neurons to remain free from pain,” Ji said.
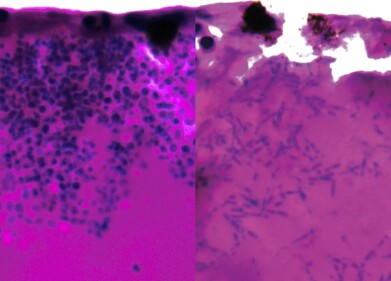
When the researchers enhanced this energy exchange in mice, pain-related behaviours fell by as much as 50 per cent. The team also tested a more direct strategy by injecting isolated mitochondria into the dorsal root ganglia, clusters of sensory neurons that transmit signals to the brain.
Mitochondria derived from healthy human or mouse donors produced comparable pain relief, whereas mitochondria taken from people with diabetes had no measurable effect, which underlined the importance of mitochondrial quality.
The study also identified a protein called MYO10 as essential for the formation of tunnelling nanotubes, without which mitochondrial transfer could not occur. Ji carried out the work with lead author Dr. Jing Xu, a research scholar in the Department of Anaesthesiology, and long-standing collaborator Professor Cagla Eroglu, a specialist in cell biology at Duke University School of Medicine with recognised expertise in glial cell behaviour.
The authors noted that further research is required, including high-resolution imaging, to confirm precisely how these nanotubes operate in living nerve tissue. Even so, the findings have highlighted a previously overlooked communication pathway between neurons and glial cells, one that could enable future therapies to address chronic pain at its biological source rather than merely suppressing symptoms.
For further reading please visit: 10.1038/s41586-025-09896-x
Digital Edition
Lab Asia Dec 2025
December 2025
Chromatography Articles- Cutting-edge sample preparation tools help laboratories to stay ahead of the curveMass Spectrometry & Spectroscopy Articles- Unlocking the complexity of metabolomics: Pushi...
View all digital editions
Events
Jan 21 2026 Tokyo, Japan
Jan 28 2026 Tokyo, Japan
Jan 29 2026 New Delhi, India
Feb 07 2026 Boston, MA, USA
Asia Pharma Expo/Asia Lab Expo
Feb 12 2026 Dhaka, Bangladesh