Research news
McMaster and MIT unveil selective antibiotic with AI-predicted mechanism against inflammatory bowel disease
Oct 16 2025
Scientists at McMaster University and the Massachusetts Institute of Technology have discovered a novel antibiotic to target inflammatory bowel disease and – in a global first – used artificial intelligence to predict how the compound works
Researchers at McMaster University in Canada, working with the Massachusetts Institute of Technology (MIT), have reported the discovery of a novel antibiotic to treat inflammatory bowel disease (IBD), alongside the successful application of artificial intelligence (AI) to predict the compound’s mechanism of action. Both outcomes represent milestones in drug discovery and clinical research.
“This work shows that we are still just scratching the surface as far as AI-guided drug discovery goes,” said Dr. Jon Stokes, assistant professor in McMaster’s Department of Biochemistry and Biomedical Sciences and principal investigator of the study.
“The development of our drug – which is designed to target IBD – has been fast-tracked thanks to collaboration between human expertise and generative AI,” he added.
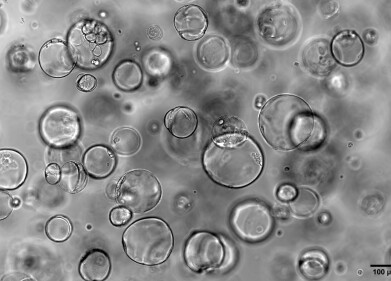
The antibiotic, named enterololin, was described as a ‘narrow-spectrum’ treatment that selectively targeted bacteria in the Enterobacteriaceae family, including Escherichia coli, while sparing the wider gut microbiome. Existing antibiotics typically operate as ‘broad-spectrum’ drugs, which eradicate beneficial bacteria as well as pathogens, thereby creating opportunities for resistant organisms to colonise the intestine. Enterololin has been designed to avoid this drawback, offering a targeted approach to manage conditions such as IBD or Crohn’s disease.
“This drug is a promising treatment candidate for the millions of patients living with IBD. We currently have no cure for conditions like these, so to develop a candidate that may alleviate symptoms significantly could help people achieve a much higher quality of life,” Stokes said.
Antibacterial compound found: McMaster team discovers wholly new class of antibiotics
The last time a new class of antibiotics reached the market was almost three decades ago – but that could soon change, thanks to a discovery by researchers at McMaster University, Hamilton, Ont... Read More
A central advance of the research lay in AI’s role. Until now, computational methods in drug discovery have largely predicted which molecules may show therapeutic activity but they have not offered insight into how those molecules exert their effect.
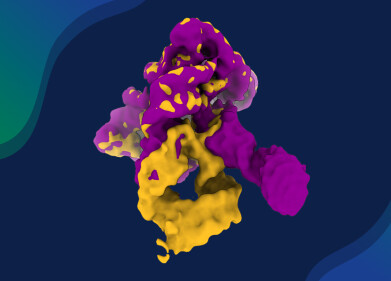
The Stokes group, in collaboration with colleagues at MIT’s Computer Science and Artificial Intelligence Laboratory, deployed an AI platform called DiffDock. In 100 seconds, the model predicted that enterololin targeted a protein complex known as LolCDE, essential for the survival of certain bacteria.
“What we are showing here is that AI can provide mechanistic explanations which are critical to move a molecule through the development pipeline,” said Dr. Regina Barzilay, a professor at MIT’s School of Engineering and developer of DiffDock, who has been named among Time magazine’s most influential figures in AI.
Validation remained essential, and Stokes’ team, led by McMaster doctoral researcher Denise Catacutan, confirmed the AI prediction through standard mechanism of action (MOA) studies.
“We did all of our standard MOA workup to validate the prediction – to see if the experiments would back up the AI – and they did. Doing it this way shaved around 18 months off our usual timeline,” Catacutan said.
Stokes estimated that MOA studies typically take two years and cost more than $2 million. In this case, the work was completed in six months at a cost of $60,000. The capacity to accelerate both timelines and cost structures highlights the potential of AI not only to generate candidates but to streamline resource-intensive phases of drug development.
“Drug resistance and our lack of new candidate drugs is a leaky faucet,” Stokes said.
“You can leave it be for a while, but eventually you will face a major problem. AI is my wrench – a tool to fix the leak before it becomes a flood. My focus is on getting new drugs to the patients who need them, and as long as AI can help me do that, I will continue to explore new ways to use it,” he added.
Enterololin has already been licensed to Stoked Bio, a spin-out company led by Stokes. The company is currently optimising the compound for human use and testing modified variants against other resistant pathogens, including Klebsiella species.
“The identification of enterololin underscores the remarkable science emerging at McMaster. We are proud to partner with the university to translate this breakthrough into real therapies for patients,” said Jeff Skinner, chief executive officer at Stoked Bio. If preclinical progress continues, enterololin may advance to human trials within three years.
“Working on something translational like this is surreal. The fact that something we discovered in the lab may one day help patients is truly amazing and reinforces the significance of our work,” concluded Catacutan.
For further reading please visit: 10.1038/s41564-025-02142-0
Digital Edition
Lab Asia Dec 2025
December 2025
Chromatography Articles- Cutting-edge sample preparation tools help laboratories to stay ahead of the curveMass Spectrometry & Spectroscopy Articles- Unlocking the complexity of metabolomics: Pushi...
View all digital editions
Events
Jan 21 2026 Tokyo, Japan
Jan 28 2026 Tokyo, Japan
Jan 29 2026 New Delhi, India
Feb 07 2026 Boston, MA, USA
Asia Pharma Expo/Asia Lab Expo
Feb 12 2026 Dhaka, Bangladesh