News
Experimental mRNA therapy shows preclinical promise to combat antibiotic-resistant pneumonia
Dec 05 2025
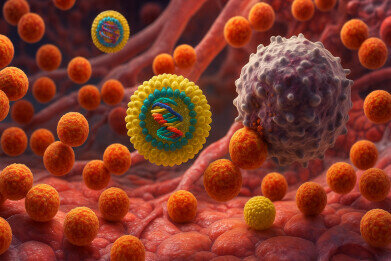
A messenger RNA therapy that instructs the body to produce a bacteria-killing 'peptibody' has shown early success in mouse and human lung models of multidrug-resistant pneumonia, in work that could pave the way for a versatile platform against infections that evade current antibiotics
Researchers at the Icahn School of Medicine at Mount Sinai, New York, US have reported early preclinical success with an mRNA-based therapy designed to combat antibiotic-resistant bacteria. The work has provided a proof of principle that an mRNA-encoded antimicrobial agent can both kill bacteria and enhance host immunity in models of multidrug-resistant pneumonia.
In mouse model studies, and in experiments with human lung tissue ex vivo, the investigational therapy slowed bacterial growth, strengthened immune cell activity, and reduced lung tissue damage. The researchers focused on multidrug-resistant Staphylococcus aureus and Pseudomonas aeruginosa, two major causes of hospital-acquired and ventilator-associated pneumonia. These pathogens have posed particular challenges because they often carry multiple resistance mechanisms that render standard antibiotic regimens only partially effective or ineffective.
Antibiotic-resistant infections are a major and growing global threat. They are estimated to kill more than 1.2 million people each year and to contribute to nearly 5 million deaths worldwide. In the US alone, more than 3 million such infections occur annually, causing up to 48,000 deaths and imposing healthcare costs that run into billions of dollars. Experts have warned that resistance has increased across nearly all major bacterial species, with the increasing possibility that routine surgery, many cancer treatments, organ transplantation and intensive care for premature infants may face infections that clinicians may not be able to reliably treat in the near future.
The Mount Sinai-led team has explored a different strategy from conventional drug discovery, which has usually sought to identify small-molecule antibiotics that directly attack bacterial targets. Their experimental therapy has delivered mRNA that instructs the patient’s own cells to produce a specialised infection-fighting protein known as a 'peptibody'. This engineered molecule combines features of an antimicrobial peptide, which can disrupt bacterial membranes, with an antibody-like domain that can bind and help direct immune responses.
At the infection site, the ‘peptibody’ is intended to perform two complementary roles. It can directly damage and kill harmful bacteria, and it can also recruit and activate immune cells to clear the remaining organisms. By design, the approach aims to support and amplify innate and adaptive immunity rather than rely solely on the direct bactericidal effect of a drug molecule.
To deliver the mRNA safely and efficiently, the investigators encapsulated it lipid nanoparticles (LNPs). This technology which underpinned the mRNA vaccines designed for Sars-COV-2 – the coronavirus that caused COVID-19 – protects the mRNA during transit in the bloodstream and facilitate its entry into target cells. In this study, the LNPs also carried an additional component that helped to limit harmful inflammation by neutralising excess reactive oxygen species, highly reactive molecules that the body produces during infection and that can damage host tissues and exacerbate symptoms in severe, hard-to-treat infections.
In mouse models of multidrug-resistant S. aureus and P. aeruginosa pneumonia, repeated doses of the mRNA–peptibody formulation were well tolerated. Treatment reduced bacterial numbers in the lungs, lowered levels of inflammatory markers, and preserved normal lung architecture when compared with control animals. According to the report, histological examination showed less oedema, less cellular infiltration, and fewer structural distortions in treated mice.
Experiments with human lung tissue obtained from donors provided further evidential support. The authors exposed the tissue to multidrug-resistant bacteria in the laboratory and then applied the therapy. They observed reduced bacterial growth and evidence that the peptibody could function alongside human immune cells, which suggested that the mechanism of action may translate beyond animal models. These ex vivo studies have strengthened the biological rationale for further development.
“‘Our work suggests there may be a novel path to tackle antibiotic-resistant infections by supporting the immune system more directly,’ said Dr. Xucheng Hou, a lead author of the study and assistant professor of immunology and immunotherapy in the laboratory of Dr. Yizhou Dong, at the Icahn School of Medicine at Mount Sinai.
“Although we are still in the early stages and have only tested this approach in preclinical models, the results have laid important groundwork for future therapies that could enhance how traditional antibiotics perform,” he added.
The authors have emphasised that the platform nature of mRNA technology could allow relatively rapid retargeting of peptibodies against different bacterial species or resistance profiles. In principle, only the encoded sequence would need to change, while the delivery system could remain largely the same.
Next, the researchers intend to continue preclinical studies and to refine dosing strategies, safety profiles and combinations with existing antibiotics. Should these studies also prove to be successful, the programme would move towards early-phase clinical trials in humans to evaluate safety, pharmacokinetics, immune responses and preliminary signals of efficacy. However, regulatory agencies are expected to scrutinise such therapies closely, given the relatively short clinical experience with mRNA platforms outside vaccination.
“‘This was the first evidence that an mRNA-encoded antimicrobial peptide could directly kill bacteria while also turning on the immune system’s protective responses,’ said Dr Dong, the senior and co-corresponding author of the study, Mount Sinai professor in nanomedicine and a member of the Icahn Genomics Institute and the Marc and Jennifer Lipzhultz Precision Immunology Institute (PrIISM) at the Icahn School of Medicine at Mount Sinai.
‘If future studies bear this out, it could open the door to a highly adaptable platform for the development of novel treatments against infections that no longer respond to today’s antibiotics,” he concluded.
Although the approach remains at an early experimental stage, the work has added to a growing body of research that aims to harness mRNA technologies beyond vaccination. If mRNA–peptibody therapies prove safe and effective in humans, they could form part of a broader toolkit to manage antimicrobial resistance, alongside existing stewardship programmes, rapid diagnostics and the rationing of use of existing drugs.
For further reading please visit: 10.1038/s41587-025-02928-x
Digital Edition
Lab Asia Dec 2025
December 2025
Chromatography Articles- Cutting-edge sample preparation tools help laboratories to stay ahead of the curveMass Spectrometry & Spectroscopy Articles- Unlocking the complexity of metabolomics: Pushi...
View all digital editions
Events
Jan 21 2026 Tokyo, Japan
Jan 28 2026 Tokyo, Japan
Jan 29 2026 New Delhi, India
Feb 07 2026 Boston, MA, USA
Asia Pharma Expo/Asia Lab Expo
Feb 12 2026 Dhaka, Bangladesh