News
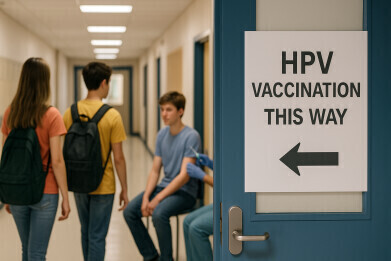
One-in-three US adults unaware of link between human papillomavirus and six types of cancer
Aug 21 2025
A research teams from the MUSC Hollings Cancer Center (Hollings), Charleston, South Carolina, has discovered that a considerable proportion of US adults remain ignorant of the connection between human papillomavirus (HPV) and multiple forms of cancer – HPV can cause six types of cancer – it is responsible for almost all cases of cervical cancer, accounts for the majority of oropharyngeal (throat) cancers and also significantly contributes to the number of cases of anal, vaginal, vulvar and penile cancers each year.
Awareness of the HPV virus as a causal link is vital, explained lead researcher Kalyani Sonawane, PhD, because it should better inform decisions about made childhood vaccination against HPV prior to the person becoming sexually active.
“When people make decisions about whether they want to get vaccinated or whether they want to get their child vaccinated, they are doing a risk-versus-benefit assessment. So it’s important for them to understand what can happen when someone gets an HPV infection,” she said.
Broadly, without the intervention of an HPV vaccination programme, it is estimated that 75–80 per cent of sexually active Americans will be infected with HPV at some point in their lifetime. And that more than 80 percent of American women are expected to contract at least one genital HPV strain by the age of 50.
Sonawane and colleagues analysed data from the Health Information National Trends Survey (HINTS), a survey conducted by the US National Cancer Institute.
The analysis revealed that about a third of people nationwide were unaware of either HPV or the HPV vaccine. The lack of awareness tended to cluster in states in the Midwest and the South. And in 13 states more than 40 per cent of people were unaware that there is a vaccine against HPV.
The vaccine remains the first and best defence against cancers caused by HPV. Research from Europe and the United States – including work at Hollings – has demonstrated a significant reduction in cervical cancer cases among young women. The young women of today were children when the vaccine was first introduced and therefore constitute the first cohort to have received it. As they age into the decades when development of the cancers is most prevalent, scientists expect to observe even greater reductions in HPV-related cancers.
Cervical cancer has served as the bellwether, because that type of cancer most commonly manifests in people in their 30s or 40s. Oropharyngeal cancers, by contrast, are most often diagnosed in people in their 50s or 60s, so it will take some time before the first vaccinated cohort reaches that age.
Sonawane noted that the greatest knowledge gap relates to oropharyngeal cancer. Across the nation, 70 per cent of those who had heard about HPV did not know that it causes oropharyngeal cancer.
“HPV is linked with six different types of cancers, but cervical cancer seems to be the one that people most know,” she said. That, she suggested, probably goes back to the original introduction of the vaccine in 2006.
“It was first approved for girls and heavily marketed toward girls. Even the packaging was pink.”
Though the vaccine has since been approved for boys, vaccination rates among boys remain lower than among girls.
“People think, ‘Oh, cervical cancer. I don’t need to get my boys vaccinated,’” said Sonawane.
“Anecdotally, when we speak with paediatricians, they always tell us that when they ask a parent of a male child about HPV vaccination, the parents always say, ‘Oh, but he’s a boy.’”
The COVID-19 pandemic disrupted many preventive-care measures, including HPV vaccination and screening for cervical, breast and colon cancers. A recent report by the American Cancer Society indicated that screening for breast and colon cancers has since recovered. Cervical-cancer screening and HPV vaccination, however, have not.
“It worries me [what] this is going to translate [into in] five years, or 10 years down the line,” Sonawane added.
“We are losing that critical opportunity of being able to vaccinate kids (before they become sexually-active and at risk from sex as a transmission vector), being able to screen women at the right time and being able to catch these cancers early. Both primary and secondary prevention are suffering.”
The United Kingdom’s school-based HPV vaccination programmes were introduced in 2008, initially also targeting only girls aged 12–13 in England, Wales, Scotland and Northern Ireland, with catch-up campaigns for older girls. The early focus reflected the vaccine’s primary aim of preventing cervical cancer, which is almost entirely caused by HPV infection.
The first vaccine used was Cervarix, replaced in 2012 by Gardasil for its additional protection against genital warts.
Over time, growing evidence of HPV’s role in the other five cancers led to a reconsideration of the girls-only policy. Targeted vaccination for men who have sex with men was introduced first – in 2016 in Northern Ireland and in 2018 in England – and offered through sexual health and HIV clinics.
In 2019, all four UK nations expanded the school programme to include boys aged 12–13. This shift toward gender-neutral vaccination aimed to protect boys directly from HPV-related disease and to strengthen herd immunity across the population.
Scotland’s programme has been distinguished by consistently high uptake, exceeding 90 per cent for all doses, and in 2025 public health officials have reported there have been no cases (so far) of cervical cancer in fully vaccinated women. England and Wales achieved strong coverage before the COVID-19 pandemic – about 88 per cent of girls and 71 per cent of boys – but rates have since fallen to around 73 per cent and 68 per cent respectively.
Although the broad structure of the school-based programme is now similar across the devolved nations, with vaccination typically delivered in secondary school year groups by NHS teams, Scotland’s early and sustained high coverage contrasts with the more marked post-pandemic declines in England and Wales. Northern Ireland’s uptake levels remain relatively robust, though full data for boys are still emerging.
For further reading please visit: 10.1001/jamaoncol.2025.2638
Digital Edition
Lab Asia Dec 2025
December 2025
Chromatography Articles- Cutting-edge sample preparation tools help laboratories to stay ahead of the curveMass Spectrometry & Spectroscopy Articles- Unlocking the complexity of metabolomics: Pushi...
View all digital editions
Events
Jan 21 2026 Tokyo, Japan
Jan 28 2026 Tokyo, Japan
Jan 29 2026 New Delhi, India
Feb 07 2026 Boston, MA, USA
Asia Pharma Expo/Asia Lab Expo
Feb 12 2026 Dhaka, Bangladesh