-
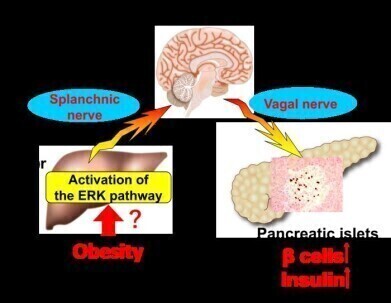 The neuronal relay system originating in hepatic ERK activation, consisting of afferent splanchnic nerves from the liver to the brain and efferent vagal nerves from the brain to the pancreas that promotes adaptive β-cell proliferation during obesity development. Credit: ©Junta Imai et al.
The neuronal relay system originating in hepatic ERK activation, consisting of afferent splanchnic nerves from the liver to the brain and efferent vagal nerves from the brain to the pancreas that promotes adaptive β-cell proliferation during obesity development. Credit: ©Junta Imai et al.
Research news
Colonic inflammation is key trigger linking obesity and insulin-producing β-cell growth in pancreas
Jun 09 2025
Scientists at Tohoku University Graduate School of Medicine have identified colonic inflammation as a previously unrecognised initiating factor in the chain of events that leads to increased insulin production in individuals with obesity. The findings, published this week, reveal a novel role for the gastrointestinal tract in regulating blood glucose levels, and could inform the development of future treatments for diabetes.
The study builds on the researchers’ previous work investigating the hepatic ERK signalling pathway – a liver-based mechanism that ultimately increases insulin secretion by pancreatic β-cells. Their latest research has traced this pathway further upstream, pinpointing inflammation in the colon – itself a consequence of obesity – as the first step in this inter-organ signalling process.
Insulin, secreted by β-cells in the pancreas, enables cells to absorb glucose from the bloodstream. In obesity, cells often become resistant to insulin, prompting the pancreas to produce more of the hormone to compensate. This increase is regulated through a neuronal signal relay that originates in the hepatic ERK pathway. With obesity so closely associated with the development of type 2 diabetes, understanding the earliest stages of this process is a critical research priority.
“The goal of this study was to define how obesity in particular triggers this cascade,” said Dr Junta Imai of Tohoku University.
“We theorised that inflammation in the colon could be a primary driver, as pro-inflammatory factors are known to activate the hepatic ERK pathway,” they said.
To test this hypothesis, the researchers conducted a series of experiments. In one, non-obese mice were administered a drug to induce inflammation in the colon. The team observed that this alone was sufficient to activate the hepatic ERK pathway, stimulate the neuronal relay system, and increase β-cell numbers – even in the absence of obesity. In a separate trial using obese mice fed a high-calorie diet, the same combination of colonic inflammation, ERK activation in the liver, and β-cell proliferation was evident.
One of the most promising findings came when the researchers treated colon inflammation in obese mice. “When we reduced inflammation in the colon, activation of the ERK pathway in the liver ceased – despite the mice remaining obese,” said Dr Imai.
“This shows that inflammation, not obesity per se, is the key factor triggering the pathway,” they concluded.
The study presents compelling evidence that the liver senses obesity via inflammatory signals from the colon, and that this colonic inflammation is the first event leading to the expansion of insulin-producing β-cells. These insights could significantly improve our understanding of how the body maintains glucose homeostasis and open new avenues for the prevention and treatment of diabetes.
The research team anticipates that their findings will help shape new therapeutic strategies targeting the gastrointestinal tract, aiming to disrupt the pathological cascade at its source before it leads to insulin resistance or diabetes.
For further reading please visit: 10.1172/jci.insight.183864
Digital Edition
Lab Asia Dec 2025
December 2025
Chromatography Articles- Cutting-edge sample preparation tools help laboratories to stay ahead of the curveMass Spectrometry & Spectroscopy Articles- Unlocking the complexity of metabolomics: Pushi...
View all digital editions
Events
Jan 21 2026 Tokyo, Japan
Jan 28 2026 Tokyo, Japan
Jan 29 2026 New Delhi, India
Feb 07 2026 Boston, MA, USA
Asia Pharma Expo/Asia Lab Expo
Feb 12 2026 Dhaka, Bangladesh