-
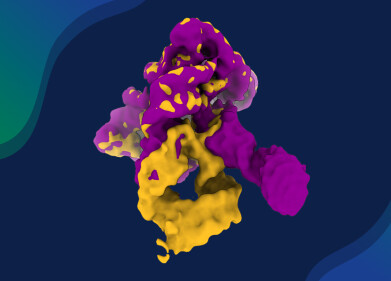
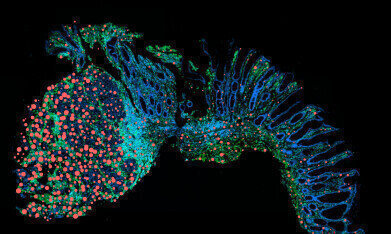 Drivers of cancer development: the inflammatory messenger oncostatin M increasingly observed in the vicinity of tumors (red), less so in healthy intestinal tissue with a normal cell structure (right). Credit: © 2025 Charité | Ahmed Hegazy
Drivers of cancer development: the inflammatory messenger oncostatin M increasingly observed in the vicinity of tumors (red), less so in healthy intestinal tissue with a normal cell structure (right). Credit: © 2025 Charité | Ahmed Hegazy
Research news
Preventing chronic inflammation from progressing to cancer of the bowel
Jul 17 2025
Charité researchers identify new therapeutic target for inflammatory bowel disease
Researchers at Charité - Universitätsmedizin, Berlin, Germany have identified a key signalling interaction that could prevent chronic intestinal inflammation from developing into cancer. The findings offer hope for more effective and personalised treatment options for people with inflammatory bowel disease (IBD), particularly young adults.
Chronic inflammatory bowel diseases – such as Crohn’s disease and ulcerative colitis – can emerge between the ages of 15 and 29. These diseases are characterised by persistent or relapsing inflammation of the gastrointestinal tract, with symptoms that include abdominal pain, diarrhoea, fatigue, weight loss and emotional distress. Long-term inflammation can damage intestinal tissue and significantly increase the risk of colorectal cancer.
Current treatments aim to suppress the immune system broadly or to block specific inflammatory signals. However, not all patients respond adequately, underscoring the need for targeted approaches. Professor Ahmed Hegazy and his team at the Department of Gastroenterology, Infectiology and Rheumatology at Charité have now uncovered a key mechanism: the interaction between two immune system messengers, interleukin-22 and oncostatin M.
Interleukin-22 supports the integrity of the gut lining, while oncostatin M is involved in tissue repair and cell signalling. The researchers found that in chronic IBD, these two proteins act together to worsen inflammation. Interleukin-22 increases the number of receptors for oncostatin M on intestinal cells, making the tissue more responsive to its pro-inflammatory effects. This feedback loop intensifies the immune response and drives further damage.
“In patients with high levels of oncostatin M, we often see a lack of response to common therapies,” said Professor Hegazy.
“This molecule could serve both as a biomarker for severe disease and a therapeutic target,” he said.
In experimental models, blocking the oncostatin M receptor significantly reduced inflammation and cancer formation.
The researchers also examined tissue samples from individuals with colorectal cancer linked to chronic inflammation. They found a high concentration of oncostatin M receptors in tumour regions, but not in adjacent healthy tissue – suggesting that this signalling pathway may contribute to cancer development in some patients.
“Chronic inflammatory bowel diseases are highly individual in their presentation and progression,” explained Professor Britta Siegmund, Director of the Clinic for Gastroenterology, Infectiology and Rheumatology.
“By identifying the amplifying effect of oncostatin M and interleukin-22, we have gained crucial insight into what drives inflammation in certain patients. This opens the door to new, more precise treatment strategies.”
A clinical trial is now underway to test an antibody therapy that blocks the oncostatin M receptor, with the aim of halting the harmful immune response while preserving the gut’s natural defences.
For further reading please visit: 10.1038/s41590-025-02149-z
Digital Edition
Lab Asia Dec 2025
December 2025
Chromatography Articles- Cutting-edge sample preparation tools help laboratories to stay ahead of the curveMass Spectrometry & Spectroscopy Articles- Unlocking the complexity of metabolomics: Pushi...
View all digital editions
Events
Jan 21 2026 Tokyo, Japan
Jan 28 2026 Tokyo, Japan
Jan 29 2026 New Delhi, India
Feb 07 2026 Boston, MA, USA
Asia Pharma Expo/Asia Lab Expo
Feb 12 2026 Dhaka, Bangladesh