-
-
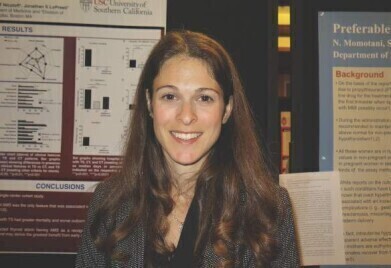 Dr Melissa Lechner. CreditL M Lechner
Dr Melissa Lechner. CreditL M Lechner
Research news
Autoimmune drugs may reverse or prevent type 1 diabetes related to immunotherapy
Jul 31 2025
A class of existing autoimmune drugs may offer a novel strategy to prevent or reverse a rare but serious complication of cancer immunotherapy, according to researchers at the UCLA Health Jonsson Comprehensive Cancer Centre.
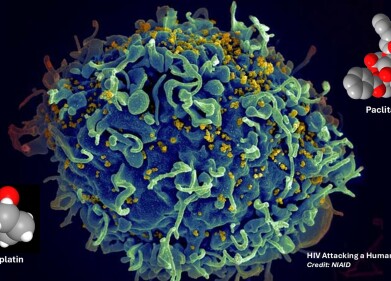
The study has identified a previously unrecognised population of immune cells involved in the development of immune checkpoint inhibitor–induced type 1 diabetes. The team demonstrated in preclinical models that Janus kinase (JAK) inhibitors – which are a class of drug already authorised for clinical use in conditions such as psoriasis and rheumatoid arthritis – could halt the autoimmune destruction of insulin-producing beta cells in the pancreas. In some instances, the intervention even appeared to reverse the damage and restore glucose regulation.
Checkpoint inhibitors, including pembrolizumab and nivolumab, have transformed cancer treatment by harnessing the immune system to target tumours. However, they have also been associated with serious immune-related adverse effects. Type 1 diabetes, although affecting only 1–2% of patients, is among the most severe: nearly 90% of those affected require intensive care for acute complications and are left permanently insulin-dependent.
To investigate the underlying mechanisms of this adverse effect, Dr Melissa Lechner and colleagues used murine models to identify the responsible immune cell subsets. They found that CD4+ T follicular helper (Tfh) cells, rather than the more commonly implicated CD8+ T cells, played a central role in driving the autoimmune response. These cells secrete interleukin-21 (IL-21) and interferon-gamma (IFNγ), both of which contribute to beta cell destruction.
By administering JAK inhibitors, which disrupt IL-21 and IFNγ signalling, the researchers successfully prevented disease onset and reduced the number of pathogenic Tfh cells. In some animals, normal glycaemic control returned, suggesting the intervention could be used both preventatively and therapeutically.
“This is the first study to identify Tfh cells and the IL-21/IFNγ axis as principal drivers of checkpoint inhibitor–induced type 1 diabetes,” said Lechner, assistant professor of medicine in endocrinology, diabetes, and metabolism at the David Geffen School of Medicine at UCLA, California.
“Crucially, we showed that this pathway can be targeted using an already approved drug, without impairing the immune system’s ability to combat cancer,” she said.
The group had previously linked the same Tfh cell population to checkpoint inhibitor–induced thyroid toxicity, suggesting a possible shared pathway for various autoimmune complications.
“These CD4+ T cells appear to play a common role in multiple immunotherapy-associated toxicities,” said Lechner.
“They could potentially serve as a biomarker to identify high-risk patients before symptoms emerge,” she added.
The team is currently preparing a first-in-human clinical trial to evaluate the approach in patients who develop diabetes after cancer immunotherapy.
Lechner stated that if proven safe and effective, this strategy could widen the use of immunotherapy by enabling access for patients with pre-existing autoimmune disease, who are typically excluded from trials.
“We hope this work will help to mitigate long-term toxicities and offer lasting solutions for patients who are now living with permanent consequences,” she said.
For further reading please visit: 10.1172/jci.insight.188843
Digital Edition
Lab Asia Dec 2025
December 2025
Chromatography Articles- Cutting-edge sample preparation tools help laboratories to stay ahead of the curveMass Spectrometry & Spectroscopy Articles- Unlocking the complexity of metabolomics: Pushi...
View all digital editions
Events
Jan 21 2026 Tokyo, Japan
Jan 28 2026 Tokyo, Japan
Jan 29 2026 New Delhi, India
Feb 07 2026 Boston, MA, USA
Asia Pharma Expo/Asia Lab Expo
Feb 12 2026 Dhaka, Bangladesh