-
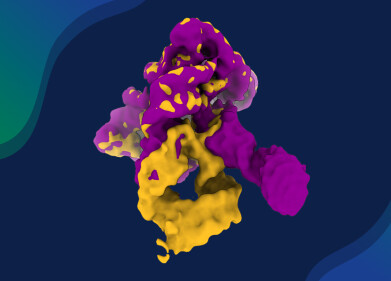
 TTFields device, which delivers targeted waves of electric fields directly into tumours to stop their growth and signal the body’s immune system to attack cancerous tumour cells. Credit: Novocure GmbH
TTFields device, which delivers targeted waves of electric fields directly into tumours to stop their growth and signal the body’s immune system to attack cancerous tumour cells. Credit: Novocure GmbH
Research news
Could electric fields supercharge immune attack on the deadliest form of brain cancer
Jun 23 2025
Electric field device placed on the scalp, along with immunotherapy and chemotherapy, may help patients with glioblastoma live longer – particularly those with large, inoperable tumours
Researchers at Keck Medicine of University of Southern California, Los Angeles, may have uncovered an effective combination therapy for glioblastoma, a brain tumour diagnosis which offers few effective treatments. According to the US National Brain Tumour Society, the average survival for patients diagnosed with glioblastoma is eight months.
The study found that using Tumour Treating Fields therapy (TTFields) to deliver targeted waves of electric fields directly into tumours to prevent growth – and also to signal the body’s immune system to attack cancerous cells – may extend survival among patients when combined with an immunotherapy, pembrolizumab, and the chemotherapy temozolomide.
TTFields disrupt tumour growth with low-intensity, alternating electric fields that push and pull vital structures inside tumour cells in continually shifting directions, making it difficult for the cells to multiply. Preventing tumour growth improves patients’ chances of recovering from the cancer.
When treating glioblastoma, TTFields are delivered through a set of mesh electrodes (pictured) positioned on the scalp to generate fields at a precise frequency and intensity focused on the tumour. Patients wear the electrodes for around 18 hours a day.
Researchers observed that TTFields attract more tumour-fighting T cells into and around the glioblastoma. Follow-up with immunotherapy keeps these T cells active for longer, replacing them with even stronger, more effective cells.
“By using TTFields with immunotherapy, we prime the body to mount an attack on the cancer, enabling immunotherapy to have a meaningful effect in ways it could not before.
“Our findings suggest that TTFields may be the key to unlocking the value of immunotherapy in treating glioblastoma,” said Dr. David Tran, MD, PhD, chief of neuro-oncology with Keck Medicine, co-director of the USC Brain Tumour Centre and corresponding author of the study.
TTFields are commonly combined with chemotherapy in cancer treatment. However, even with aggressive treatment, the prognosis for glioblastoma remains poor. Although immunotherapy has proven successful in several other cancer types, it has not been effective on its own in treating glioblastoma.
In this study, adding immunotherapy to TTFields and chemotherapy was associated with a 70% increase in overall survival. Patients with larger, unresected tumours experienced an even stronger immune response and lived longer, suggesting that a greater tumour burden may provide more targets for the therapy.
Pembrolizumab, an immune checkpoint inhibitor, enhances the body’s natural ability to fight cancer by improving T cells’ capacity to identify and attack malignancies. The relative scarcity of T cells in and around glioblastomas has been attributed to the tumours originating in the brain and being shielded by the blood–brain barrier, which tightly regulates cell and substance entry from the bloodstream.
This immunosuppressive environment reduces the effectiveness of standard therapies such as pembrolizumab and chemotherapy. Tran theorised that initiating an immune reaction directly within the tumour – an approach known as ‘in situ immunisation’ using TTFields – may overcome this issue.
The study, which analysed data from the Phase 2 clinical trial 2-THE-TOP, enrolled 31 newly diagnosed glioblastoma patients who had completed chemoradiation therapy. Of these, 26 received TTFields combined with both chemotherapy and immunotherapy. Seven of the 26 patients had inoperable tumours owing to their locations.
Patients received six to 12 monthly treatments of chemotherapy alongside TTFields for up to 24 months, while immunotherapy was administered every three weeks starting with the second chemotherapy dose for up to 24 months. Compared with previous patients using TTFields with chemotherapy alone, those in this trial lived approximately 10 months longer, and patients with large, inoperable tumours lived about 13 months longer with a notably stronger immune activation response.
Further studies are needed to determine the optimal role of surgery in this setting, but these findings may offer hope, particularly for glioblastoma patients for whom surgery is not an option.
Keck Medicine is participating in a multicentre Phase 3 clinical trial to validate the efficacy of TTFields with immunotherapy and chemotherapy. Tran, who has researched TTFields for more than a decade, chairs the trial's steering committee.
The trial is currently open at 28 sites across the United States, Europe and Israel and aims to enrol over 740 patients through April 2029 to assess how surgical resection influences the immune response.
For further reading please visit: 10.1016/j.medj.2025.100708
Digital Edition
Lab Asia Dec 2025
December 2025
Chromatography Articles- Cutting-edge sample preparation tools help laboratories to stay ahead of the curveMass Spectrometry & Spectroscopy Articles- Unlocking the complexity of metabolomics: Pushi...
View all digital editions
Events
Jan 21 2026 Tokyo, Japan
Jan 28 2026 Tokyo, Japan
Jan 29 2026 New Delhi, India
Feb 07 2026 Boston, MA, USA
Asia Pharma Expo/Asia Lab Expo
Feb 12 2026 Dhaka, Bangladesh