-
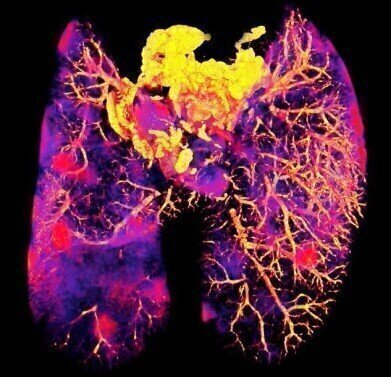 Mycobacterium tuberculosis infected mouse lung (Credit The Francis Crick Institute)
Mycobacterium tuberculosis infected mouse lung (Credit The Francis Crick Institute)
News
Imaging Method reveals whether Antibiotics reach Bacteria hiding in Tissues
Jan 15 2021
During bacterial infections such as tuberculosis, bacteria enter human cells posing a challenge for treatment, as antibiotics must reach and enter all infected cells in order to be effective. If researchers could select for or develop more effective antibiotics based on where they reach, this may reduce the length of treatment needed, which in turn could reduce the risk of antibiotic resistance developing.
Scientists at the Francis Crick Institute and the University of Western Australia have developed a new imaging method to see where in the infected tissues and in the cells, an antibiotic given to treat tuberculosis had reached the bacteria. The scientists are continuing to work on the method, adapting it for other types of antibiotic and to image multiple antibiotics at the same time.
Max Gutierrez, author and group leader of the Host-Pathogen Interactions in Tuberculosis Laboratory at the Crick, says: “In the case of tuberculosis, people need to be treated with at least three different antibiotics over six months. We don’t yet fully understand why this extended treatment is needed. We hope that being able to more clearly see where antibiotics are going, will help us better understand this process and find ways to improve it.”
The imaging method, correlative light, electron and ion microscopy in tissue (CLEIMiT) was used to analyse lung tissue from mice infected with tuberculosis and treated with the antibiotic bedaquiline.
A combination of other imaging methods, including confocal laser scanning microscopy, 3D fluorescence microscopy, electron microscopy and nanoscale secondary ion mass spectrometry, were also used to to develop the new approach.
Using this method, they found that bedaquiline had not reached all infected cells in the lung tissue and also had not entered all infected areas within infected cells.
They also found this antibiotic was collecting in macrophages and in polymorphonuclear cells, both types of immune cell. This was a surprise as these cells have different environments and it wasn’t thought that one antibiotic would be able to enter both.
Tony Fearns, author and senior laboratory research scientist in the Host-Pathogen Interactions in Tuberculosis Laboratory at the Crick, says: “Our approach could be used to help develop new antibiotics or to re-assess current antibiotics to judge how effectively they reach their targets. The more we learn about how drugs behave in the body, for example where they collect, the better we will be able to treat bacterial diseases like tuberculosis.”
Published in PLoS Biology
Digital Edition
Lab Asia Dec 2025
December 2025
Chromatography Articles- Cutting-edge sample preparation tools help laboratories to stay ahead of the curveMass Spectrometry & Spectroscopy Articles- Unlocking the complexity of metabolomics: Pushi...
View all digital editions
Events
Jan 21 2026 Tokyo, Japan
Jan 28 2026 Tokyo, Japan
Jan 29 2026 New Delhi, India
Feb 07 2026 Boston, MA, USA
Asia Pharma Expo/Asia Lab Expo
Feb 12 2026 Dhaka, Bangladesh


















