Research news
One-time CRISPR gene editing therapy targeting ANGPTL3 halves cholesterol and triglycerides in first human trial
Nov 21 2025
Early Phase 1 results from 15 adults with difficult-to-treat lipid disorders have shown that CTX310 – a one-time CRISPR-Cas9 therapy which targets ANGPTL3 in the liver – has safely cut LDL cholesterol and triglycerides
A single infusion of an investigational CRISPR-Cas9 gene-editing therapy has safely reduced low-density lipoprotein (LDL) cholesterol and triglycerides by about half in people with difficult-to-treat lipid disorders, in a first-in-human Phase 1 trial that has been presented as late-breaking science at the American Heart Association’s Scientific Sessions 2025 held in New Orleans, USA, at the beginning of November.
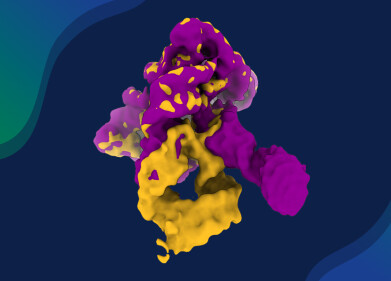
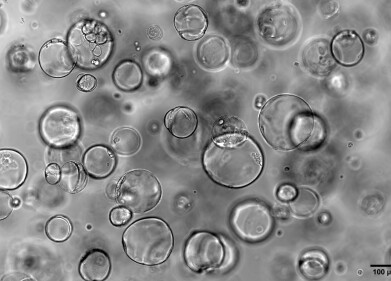
The study evaluated CTX310, an experimental therapy that uses CRISPR-Cas9 gene-editing technology to target angiopoietin-like protein 3 (ANGPTL3). CTX310 is delivered as a one-time intravenous infusion in tiny lipid nanoparticles that transport the editing machinery into liver cells.
In the liver the construct cuts the ANGPTL3 gene and disrupts its expression. ANGPTL3 normally modulates lipid metabolism; people who are born with natural loss-of-function variants in ANGPTL3 have lifelong low LDL cholesterol and triglyceride concentrations without obvious adverse effects and appear to have a lower lifetime risk of atherosclerotic cardiovascular disease. The therapeutic concept is therefore to mimic this naturally protective state through a permanent edit in liver cells.
Researchers enrolled 15 adults aged between 18 and 75 years – but with a median age of 53 years – across six sites in Australia, New Zealand and the United Kingdom. Thirteen participants were male and two were female. All participants had markedly elevated lipid levels despite maximum tolerated lipid-lowering therapy. The cohort included one person with homozygous familial hypercholesterolaemia (FH), a rare inherited disorder that causes extremely high LDL cholesterol; five with heterozygous FH; one with mixed dyslipidaemia, in which both cholesterol and triglycerides are raised; and two with severe hypertriglyceridaemia, defined as very high blood triglyceride concentrations.
CTX310 was administered as a single intravenous infusion after pre-treatment with corticosteroids and antihistamines to reduce the risk of infusion reactions. Doses ranged from 0.1 to 0.8 mg per kilogram of body weight in an ascending dose design, with participants assigned to one of five dose levels. The primary aims were to assess safety, tolerability and pharmacokinetics – how the investigational gene therapy was processed in the body – and to evaluate effects on LDL cholesterol and triglycerides.
All patients had at least 60 days of safety follow-up at the time of analysis which was cut off in September 2025. Participants will remain in the core trial for one year, with additional long-term safety follow-up for another 15 years which is the United States Food and Drug Administration (FDA) guidance for CRISPR-based therapies.
Cholesterol and triglyceride levels began to fall at two weeks following infusion. These reductions persisted for at least 60 days in all dose groups assessed to date. In the highest dose cohort, LDL cholesterol and triglycerides fell by up to 60%, and average reductions across that group approached or exceeded 50%. Investigators had considered a 30–40% reduction a clear sign of success in such an early-stage study, so the magnitude of change was larger than they had anticipated.
Notably, CTX310 has become the first reported intervention to achieve large reductions in both LDL cholesterol and triglycerides at the same time in this context which may be especially important for people with mixed lipid disorders who often have elevations in more than one lipid parameter.
“This is really unprecedented. A single treatment that simultaneously lowered LDL cholesterol and triglycerides,” said Dr. Luke J. Laffin, lead study author, a preventive cardiologist, and co-director of the Center for Blood Pressure Disorders in the Department of Cardiovascular Medicine at the Cleveland Clinic, Cleveland, Ohio, USA.
Laffin added that, if these results are confirmed in larger and longer-term trials, a one-time therapy that durably switches off ANGPTL3 could transform care for people with lifelong lipid disorders and substantially cut cardiovascular risk. The World Health Organization estimates that cardiovascular disease accounts for around 19.8 million deaths per year worldwide which is around one third of all deaths worldwide.
The findings suggest that a gene-editing strategy could, for some patients, remove the need for daily or monthly lipid-lowering medicines such as statins, ezetimibe, proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitors or triglyceride-directed agents.
Safety data from this Phase 1 trial have been reassuring so far, although the investigators emphasised that longer follow-up will be essential. Three participants experienced minor infusion-related reactions, including back pain and nausea, which resolved with standard medication. One participant who had raised liver enzymes at screening showed a temporary further increase in liver enzymes after treatment; this abnormality persisted for a few days then returned to normal without specific intervention.
No long-term or serious safety concerns have been observed to date in any participant, and intensive safety monitoring has continued. The durable change to DNA inherent in CRISPR-Cas9 technology means that regulators require extended follow-up; the FDA currently recommends up to 15 years of safety observation for individuals who receive genome-editing therapies.
“Adherence to cholesterol-lowering therapy is one of the biggest challenges in preventing heart disease,” said Dr. Steven E. Nissen, FAHA, a co-author of the study and chief academic officer at the Cleveland Clinic Heart, Vascular and Thoracic Institute.
He noted that many patients stop their cholesterol medicines within the first year of prescription, often because of side effects, treatment fatigue or misunderstanding of risk. He suggested that the prospect of a one-time infusion with durable lipid-lowering effects could represent a major clinical advance.
Further context of the potential for a therapy is a very large global burden of dyslipidaemia. High cholesterol is a major modifiable risk factor for heart attack and stroke. In response to this burden, the American Heart Association has launched the Lower Your LDL Cholesterol Now™ Initiative, a three-year national campaign to help heart attack and stroke survivors understand their LDL cholesterol, improve access to testing, and support adherence to treatment.
Investigators emphasised that the present study remains an early Phase 1 trial with several important limitations. The sample size is small and primarily male, which restricts the ability to generalise findings to women or to broader populations. All participants were adults from Australia, New Zealand and the UK, so responses in people from other regions or ethnic backgrounds remain unknown.
The cohort also included patients with a variety of lipid disorders, from different forms of familial hypercholesterolaemia to isolated hypertriglyceridaemia, which complicates interpretation of treatment effects in any single diagnostic group. Larger Phase 2 trials that enrol more diverse participants will therefore be needed to characterise efficacy and safety across different patient types and to explore effects on clinical cardiovascular outcomes such as heart attack and stroke.
“This has been a great opportunity to perform a pivotal first-in-human gene editing study of ANGPTL3 in patients in Australia and New Zealand,” said Dr. Stephen J. Nicholls, lead study investigator and director of the Victorian Heart Institute at Monash University, Melbourne, Australia. He underlined the importance of international collaboration to evaluate highly specialised therapies such as CRISPR-based gene editing, particularly when long-term follow-up is mandatory.
The trial has demonstrated that inactivation of ANGPTL3 through a single administration of CTX310 in humans is feasible, that it can lead to rapid and substantial reductions in LDL cholesterol and triglycerides, and that – in this small cohort – the approach has appeared safe in the short term. Participants follow-up will be closely scrutinise by regulators for their long-term data. Phase 2 studies are already planned for late 2025 or early 2026 and will focus on broader patient populations, extended follow-up and cardiovascular outcomes.
Digital Edition
Lab Asia Dec 2025
December 2025
Chromatography Articles- Cutting-edge sample preparation tools help laboratories to stay ahead of the curveMass Spectrometry & Spectroscopy Articles- Unlocking the complexity of metabolomics: Pushi...
View all digital editions
Events
Jan 21 2026 Tokyo, Japan
Jan 28 2026 Tokyo, Japan
Jan 29 2026 New Delhi, India
Feb 07 2026 Boston, MA, USA
Asia Pharma Expo/Asia Lab Expo
Feb 12 2026 Dhaka, Bangladesh