-

-
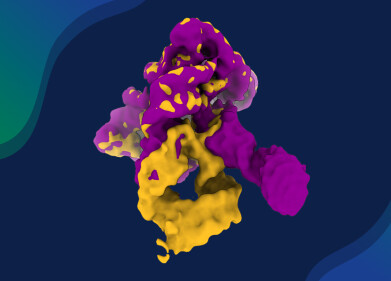
 Credit: Copyright © 2025 Lingxuan Tang et al
Credit: Copyright © 2025 Lingxuan Tang et al
Research news
Multi-target strategy proposed to tackle sepsis through treatment with dynamic pathway
Nov 12 2025
Researchers have proposed a personalised, multi-target therapeutic approach to treat sepsis by dynamically regulating key signalling pathways that control immune activation, inflammation and cellular metabolism, to reduce mortality
Research led by Professor Zou Zui of the School of Anesthesiology, Naval Medical University, Shanghai, China and his team drawn from across the Naval Medical University has provided insight into the complex biological mechanisms that drive sepsis – a life-threatening condition marked by dysregulated immune responses, systemic inflammation and multi-organ failure.
The study describes how multiple signalling pathways – including nuclear factor-kappa B (NF-κB), Janus kinase/signal transducer and activator of transcription (JAK/STAT), toll-like receptor (TLR), mitogen-activated protein kinase (MAPK), hypoxia-inducible factor-1 alpha (HIF-1α) and the Nrf2/Keap1 axis – interact to regulate immune activation, inflammation and cellular metabolism.
The researchers observed that mitochondrial dysfunction and altered metabolic processes contribute significantly to the disease by reducing energy production and impairing immune-cell function. Conventional treatment approaches, which depend mainly on antibiotics and early goal-directed therapy, can fail to achieve satisfactory outcomes. Professor Zou and his colleagues proposed that selective inhibition of key pathways may help to curb hyperinflammation and prevent organ failure.
However, they emphasised that because sepsis is dynamic and heterogeneous, single-target therapies are unlikely to succeed. Instead, they have suggested a personalised, multi-target modulatory approach that allows real-time adjustment of treatment according to signalling-pathway activity. This strategy could enable more precise regulation of inflammation, immune balance and metabolic stability while minimising side effects. The team suggested that future research should translate these mechanistic findings into clinical applications to improve prognosis through dynamic and individualised interventions.
Their work describes in detail the NF-κB pathway, in which sepsis-inducing factors such as lipopolysaccharide go on to activate toll-like receptors, initiating downstream cascades leading to the nuclear translocation of NF-κB. Once activated, NF-κB promotes transcription of pro-inflammatory cytokines including tumour necrosis factor-alpha and interleukin-1 beta, which intensify the systemic inflammatory response. The researchers also contrasted this with the NF-κB pathway, which operates through distinct kinases and co-factors and typically responds to different cellular stimuli.
The team further examined the JAK/STAT pathway, where cytokines such as interferon-gamma and interleukin-6 bind to surface receptors and activate Janus kinases. These enzymes phosphorylate STAT proteins, which then form dimers and enter the nucleus to regulate genes that control inflammation, survival and differentiation. Abnormal activation of this pathway can impair immune-cell performance, accelerate tissue injury and worsen organ dysfunction.
A two-step mechanism was also described for activation of the NLRP3 inflammasome. In the first stage, known as priming, pathogen- or damage-associated molecular patterns stimulate NLRP3 expression. The second stage involves activation through events such as potassium efflux and lysosomal rupture. The resulting inflammasome complex drives caspase-1 activation and the release of inflammatory cytokines interleukin-1 beta and interleukin-18.
Under hypoxic conditions, the team observed that the stability and activity of HIF-1α increase, leading to downstream effects on inflammation and organ function. They noted that HIF-1α interacts closely with the NF-κB pathway to amplify inflammatory responses during sepsis.
Mitochondrial processes also play a crucial role: suppression of fatty-acid oxidation reduces energy production, while impaired expression of mitochondrial transcription factor A and decreased activation of nuclear respiratory factor by peroxisome proliferator-activated receptor-gamma coactivator-1 alpha diminish mitochondrial biogenesis. These disruptions further aggravate cellular injury and energy imbalance.
The researchers concluded that sepsis remains one of the most significant challenges in global medicine, owing to its complexity, high mortality rate and variable clinical presentation. They stressed that future studies must focus on elucidating how these signalling pathways interact across different stages of disease progression. Developing precise biomarkers and personalised therapeutic strategies could, they argue, transform patient stratification and treatment outcomes.
For further reading please visit: 10.34133/research.0811
Digital Edition
Lab Asia Dec 2025
December 2025
Chromatography Articles- Cutting-edge sample preparation tools help laboratories to stay ahead of the curveMass Spectrometry & Spectroscopy Articles- Unlocking the complexity of metabolomics: Pushi...
View all digital editions
Events
Jan 21 2026 Tokyo, Japan
Jan 28 2026 Tokyo, Japan
Jan 29 2026 New Delhi, India
Feb 07 2026 Boston, MA, USA
Asia Pharma Expo/Asia Lab Expo
Feb 12 2026 Dhaka, Bangladesh