-

-
 Tess Eidem pumps allergens into a chamber to study the impact of UV light on them. Credit: Patrick Campbell/CU Boulder
Tess Eidem pumps allergens into a chamber to study the impact of UV light on them. Credit: Patrick Campbell/CU Boulder -
 Tess Eidem holds up a jar of fungus used to generate allergens for research. Credit: Patrick Campbell/CU Boulder
Tess Eidem holds up a jar of fungus used to generate allergens for research. Credit: Patrick Campbell/CU Boulder -
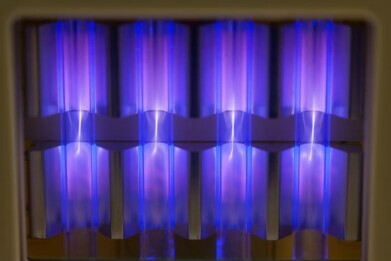 UV222 lights hang on the ceiling of the Aerobiology and Disinfection Laboratory at CU Boulder. Credit: Patrick Campbell/CU Boulder
UV222 lights hang on the ceiling of the Aerobiology and Disinfection Laboratory at CU Boulder. Credit: Patrick Campbell/CU Boulder
Laboratory news
Far-UVC light offers novel way to cut exposure to allergens in high-risk labs
Nov 17 2025
Laboratories that handle animals, plants or high-allergen materials could adapt 222-nanometre far-UVC systems to reduce the immunoreactivity of airborne proteins and support occupational health, while keeping core experimental areas free from unwanted ultraviolet effects on sensitive assays and reagents
Cats, dust mites, mould and even trees all release microscopic proteins into the air that – for people who are allergic – can provoke swollen eyes, itchy skin and impaired breathing after only the briefest of exposure. These airborne allergens can persist indoors for months after the original source has gone, and repeated exposure can worsen symptoms and can contribute to the development of asthma.
A team at the University of Colorado, Boulder, has now reported that a specific form of ultraviolet light can rapidly inactivate airborne allergens in enclosed spaces. The study has suggested a potential way to reduce the allergen burden in homes, schools and workplaces where such particles can accumulate and recirculate.
“We have found that we can use a passive, generally safe ultraviolet light treatment to quickly inactivate airborne allergens,” said study author Dr. Tess Eidem, a microbiologist senior research associate of aerobiology in the Department of Civil, Environmental and Architectural Engineering at the University of Colorado Boulder.
“We believe this could be another tool for helping people fight allergens in their home, schools or other places where allergens accumulate indoors,” she said.
The work focused on the proteins that drive allergic reactions rather than on the organisms that produce them. When a person who is sensitive to cats enters a room, the trigger is not the animal itself but airborne flecks of a protein called ‘Fel d 1’, that is found in the saliva of cat.
When cats groom, the protein transfers to shed skin and hair and then circulates as microscopic particles in the air. When a sensitised person inhales these specks of material their immune system generates antibodies that recognise the three-dimensional structure of ‘Fel d 1’ and bind to it initiating an allergic response.
Other animals and environmental sources, such as dogs, mice, dust mites, moulds and plants, release characteristic proteins of their own, each with its distinct structure for the immune system to target.
Unlike bacteria or viruses, these allergenic proteins having never been alive cannot be ‘killed’ in a conventional microbiological sense. And so they remain in carpets, furnishings and dust often long after the originating source has departed.
“After a dust mite is long gone, the allergen it produced is still there.
“That’s why, if you shake out a rug, you can have a reaction years later,” said Eidem.
Standard methods to reduce allergen levels indoors include use of a vacuum cleaner, regular washing of walls and fabrics, air filtration systems and frequent bathing of pets. These approaches can reduce exposure to some extent but require sustained effort and are difficult to maintain consistently over long periods. Previous studies have also indicated that residual allergens often remain in spite of these interventions.
Eidem, together with co-author Professor Mark Hernandez in the Department of Civil, Environmental and Architectural Engineering, and researcher Kristin Rugh, the team sought a more strategy that would apply across all types of allergen.
Instead of attempting to remove the allergens entirely, they aimed to disrupt the proteins’ three-dimensional structure so that antibodies would no longer recognise them. The approach could be described as analogous to unfolding an origami model out to a piece of paper with creases but that no longer looks like its original shape.
“If your immune system is used to a ‘swan’ but you unfold the protein, so it no longer looks like a swan, then it won’t mount an allergic response,” explained Eidem.
In this analogy, the protein’s folded structure is the ‘swan’ that the immune system has learned to identify. If light energy alters that structure, the immune response may not activate in the same way.
Ultraviolet light has already had extensive use to inactivate airborne microorganisms, including the SARS-CoV-2 virus that was the cause of the COVID-19 pandemic. Many hospitals, airports and other facilities use ultraviolet disinfection systems that emit radiation at a wavelength of about 254 nanometres. This conventional germicidal ultraviolet light is effective but can damage skin and eyes, so operators must wear protective equipment and systems usually run in unoccupied spaces.
In the present study, the Colorado group used light sources that emit at 222 nanometres. This shorter-wavelength of ultraviolet light, often referred to as far-ultraviolet C (far-UVC), does not penetrate deeply into biological tissues and has been proposed as a safer option for use in occupied environments – although some risks do remain. Eidem noted that such systems can also generate ozone and that exposure levels to this gas must be kept within safety guidelines and limits.
To test whether far-UVC could alter allergen structure in real time, the researchers introduced microscopic aerosols that contained allergens from dust mites, pet dander, mould and pollen into a sealed, unoccupied chamber with a volume of about 9.9m3. They mounted four compact UV222 lamps – approximately 20 x 25cms – on the ceiling and floor of the chamber and then activated the system.
The team sampled the air in the chamber at 10-minute intervals and compared the treated samples with original allergen-containing air (which had not been exposed to the UV light). Laboratory assays assessed how strongly antibodies bound to the proteins in each sample. In the irradiated air, immunorecognition was shown to decrease which indicated that the antibodies no longer recognised many of the proteins as effectively.
After 30 minutes of exposure to 222-nanometre light, the level of recognisable airborne allergen fell by about 20 to 25 per cent on average. This reduction did not mean that all allergens had disappeared but it did indicate a significant decline in the capacity of the aerosols to trigger an immune response.
“Those are pretty rapid reductions when you compare them to months and months of cleaning, ripping up carpet and bathing your cat,” said Eidem.
The comparison underlined the potential appeal of a technology that can operate passively in the background rather than rely solely on labour-intensive cleaning regimes.
Ultraviolet 222-nanometre (UV222) lamps are already on the market, primarily for industrial antimicrobial applications. Eidem has envisaged future portable devices that consumers could take to a friend’s home that has pets or switch on before they clear out a dusty loft or basement. The same principle could extend to workplaces where staff experience chronic exposure to allergens, such as animal facilities or indoor agriculture sites.
According to the United States Centers for Disease Control and Prevention, about one in three adults and children in the country lives with at least one allergy. For many of these individuals, respiratory allergy and asthma intertwine. Eidem emphasised that asthma attacks in the US kill about 10 people every day, often after exposure to airborne allergens.
“Trying to develop novel ways to prevent that exposure [and risk] is really important,” she said.
The work remains at an experimental stage. The study used a controlled chamber rather than occupied homes or workplaces, and the follow-up did not assess long-term health outcomes in people with allergies. Further research will be needed to confirm how far-UVC systems perform in complex real-world environments where air currents, room layouts and human activity constantly change particle distribution.
Nonetheless, the findings have added to growing interest in far-UVC as a tool to manage indoor air quality. Whereas earlier work has focused mainly on its capacity to inactivate infectious agents such as viruses and bacteria, this study has indicated that ultraviolet light at 222 nanometres can also partially neutralise non-living allergenic proteins by altering their structure. If future trials in homes, schools and workplaces support these results, ultraviolet light installations could eventually complement cleaning practices, air filtration and source control as part of a broader strategy to protect people from indoor allergens.
For further reading please visit: 10.1021/acsestair.5c00080
Digital Edition
Lab Asia Dec 2025
December 2025
Chromatography Articles- Cutting-edge sample preparation tools help laboratories to stay ahead of the curveMass Spectrometry & Spectroscopy Articles- Unlocking the complexity of metabolomics: Pushi...
View all digital editions
Events
Jan 21 2026 Tokyo, Japan
Jan 28 2026 Tokyo, Japan
Jan 29 2026 New Delhi, India
Feb 07 2026 Boston, MA, USA
Asia Pharma Expo/Asia Lab Expo
Feb 12 2026 Dhaka, Bangladesh