Abstract
Both in vivo neuropharmacology and optogenetic stimulation can be used to decode neural circuitry, and can provide therapeutic strategies for brain disorders. However, current neuronal interfaces hinder long-term studies in awake and freely behaving animals, as they are limited in their ability to provide simultaneous and prolonged delivery of multiple drugs, are often bulky and lack multifunctionality, and employ custom control systems with insufficiently versatile selectivity for output mode, animal selection and target brain circuits. Here, we describe smartphone-controlled, minimally invasive, soft optofluidic probes with replaceable plug-like drug cartridges for chronic in vivo pharmacology and optogenetics with selective manipulation of brain circuits. We demonstrate the use of the probes for the control of the locomotor activity of mice for over four weeks via programmable wireless drug delivery and photostimulation. Owing to their ability to deliver both drugs and photopharmacology into the brain repeatedly over long time periods, the probes may contribute to uncovering the basis of neuropsychiatric diseases.
Similar content being viewed by others

Main
Pharmacological manipulation of brain circuits in vivo remains one of the most extensively used and important methods for large-scale dissection of brain circuit function. Local in vivo pharmacology can render pivotal insights, not only into the roles of distinct cell types or neurochemical mechanisms for a specific physiological, cognitive or behavioural activity, but also into the understanding and treatment of various neurodegenerative diseases. In addition, local infusion of drugs over time into brain structures offers a reliable, high throughput means for developing and testing neuropharmacological compounds that can impact brain function. Recent efforts in cell-type selective control of neural circuits with optogenetics have uncovered greater specificity in the identification of translationally viable brain targets. Combinatorial use of pharmacology and optogenetics can provide specific and versatile control of neuronal populations and cells1,2,3, affording opportunities for neuroscience and clinical medicine; however, combining local pharmacology and optogenetics with spatiotemporal control using wireless methods has proven to be an arduous undertaking.
Drug infusions have conventionally been accomplished by implanting metal cannulas into the brain and connecting them to an external fluid pumping system to locally deliver pharmacological agents. However, chronic regional drug delivery and its advanced combinatorial applications with optogenetics have been significantly limited due to the use of these rigid cannulas, which can cause prolonged brain tissue damage and inflammation, and their tethered operation also restricts the animal’s natural movement4,5. For these reasons, there has been an unmet need to combine advances in materials engineering, microfluidics, optoelectronics and wireless control to pharmacologically and optically engage neuronal function in freely moving animals, alongside a chronic, stable biocompatible approach. Recent research and development have produced miniaturized, flexible, multifunctional fibres integrating fluidic channels and optical waveguides to mitigate neural tissue damage, as well as to realize the full potential of combined optogenetics and pharmacology6,7. However, these fibres still require tethered operation due to the need for multiple connections with external hardware for each modality, thus not only causing angular stress, but also hindering real time in vivo manipulation of freely moving animals in their natural environments.
To enable non-tethered neuromodulation, researchers have developed standalone neural implants using various wireless technologies (for example, infrared (IR)8,9,10,11 or radiofrequency (RF)12,13,14,15,16,17,18,19,20,21,22,23,24), however, these wireless technologies are limited due to their short operation range, line-of-sight handicaps, susceptibility to orientations and angle, requirement of special and/or bulky electronic systems, as well as limited target selectivity within a large group of animals. Additionally, current wireless technologies limit researchers in their ability to conduct multi-animal testing with a different experimental treatment for each animal in a single behavioural session. More importantly, achieving chronic in vivo pharmacology in awake, active animals is hindered by challenges to provide repeated drug delivery over an extensive timeframe using a standalone wireless neural implant8,9,14.
Here, we introduce smartphone-controlled, wireless, soft ‘plug-n-play’ optofluidic neural implants to enable ‘chronic’ in vivo neuropharmacology, together with optogenetic control schemes. This self-contained device overcomes the key limitations of current state-of-the art technologies (Supplementary Table 1) by integrating: (1) replaceable drug cartridges that can replenish drug supply with simple plug-and-play, (2) an ultrathin and soft multimodal probe that can independently deliver four distinct drugs and two different wavelengths of light to targeted areas of the deep brain and (3) a smartphone-controlled, bluetooth low energy (BLE) wireless module that features long-range coverage (10–100 m), omnidirectional access, no line-of-sight handicap, the capability for specific target selectivity and scalable closed-loop control features. This user-friendly, chronically stable design enables long-term neural circuit studies by allowing for repeated, intact pharmacological and optogenetic access to the same region with only one surgery. Our studies presented here demonstrate the innate capabilities of these plug-n-play optofluidic devices for chronic wireless in vivo pharmacology and optogenetics.
Results
Design and operation principles of a soft optofluidic probe system with replaceable plug-n-play drug cartridges
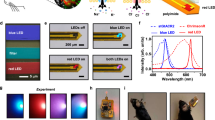
In Fig. 1a, b, we present schematic diagrams and optical micrographs of the optofluidic probe system, highlighting the plug and play based replaceable drug cartridge architecture. This cartridge-based approach allows unlimited on-demand supply of the drug without the need for repeated disruptive surgeries or replacement of the entire neural implant. The various components of the plug-n-play optofluidic system (Fig. 1a) can be grouped into two parts: (1) the replaceable male drug cartridge (blue, for chronic drug delivery) and (2) the ultrathin, soft, female adapter optofluidic probe (red, for chronic deep brain access). The male drug cartridge consists of four individual fluid reservoirs (0.5 µl), each connected to a male cartridge pillar (1.3 mm outer diameter (OD), 0.45 mm inner diameter (ID), 1.7 mm tall) and thermally actuated pumps, which can push fluid out from the reservoirs via thermal expansion of the polymer composite layer (2:1 mixture of polydimethylsiloxane (PDMS), and expandable microspheres (Expancel 031 DU 40, AkzoNobel)) through Joule heating of micro-heaters. The reservoir uses cyclic olefin polymer (COP, Zeonor 1420 R) as a structural material due to its low water vapour permeability (0.028 g mm m–2 day–1) and its inner walls have 7-µm-thick conformally coated Parylene C film (0.083 g mm m–2 day–1) to further minimize drug evaporation25. The female adapter optofluidic probe integrates a female adapter (1.5 mm thick PDMS layer with four 1.15 mm ID holes) connected to four separate microfluidic channels (each with a 10 μm × 10 μm cross-section) of a microfluidic probe (50 μm thick PDMS) with an optical layer composed of two independently controlled microscale inorganic light-emitting diodes (μ-ILEDs; blue (470 nm, TR2227, Cree Inc.) and orange (589 nm, TCE10-589, Three Five Materials)) and thin metal interconnects (5 nm/250 nm of Cr/Au) on a 6 μm thick polyethylene terephthalate (PET) film (Supplementary Fig. 1). The plug-n-play microfluidic assembly of the replaceable cartridges enables repeated, chronic drug delivery. The male pillar component of the cartridge is plugged into the female adapter structure of the microfluidic probe, such that each of the four vertical fluidic channels is self-aligned and connected to allow robust drug delivery through the microfluidic channels (Fig. 1b). Unlike previous wireless optofluidic devices, where lifespan of the device was limited to only 2 weeks post-surgery due to evaporation issues8,14, the detachable nature of the current device establishes long-term cartridge storage (−20 °C) until right before an in vivo behavioural experiment. The illustrations in Fig. 1c–f present plug-and-play operation of the optofluidic device. Following activation of a thermally actuated pump, the male cartridge pushes the fluid out of a reservoir through its pillars (Fig. 1c). When assembled with a female adapter microfluidic probe (Fig. 1d), or an optofluidic probe (Fig. 1e), the same operation delivers fluid through the plug-n-play interface into ultrathin, soft microfluidic channels. Integration of μ-ILEDs on the plug-n-play optofluidic probe makes the device highly versatile, allowing multimodal access to targeted brain circuits (Fig. 1e,f). The ultrathin, soft and flexible probe (13–18 N m–1 in bending stiffness8), together with the conceptualization of replaceable drug cartridges, facilitates minimally invasive and minimally disruptive chronic operation in awake, behaving animals. This design minimizes neural tissue damage with its biomechanical compatibility and offers a simple way to replenish drug supply on demand.
a, Exploded view of a plug-n-play optofluidic neural probe system, consisting of μ-ILEDs, a soft microfluidic probe with a female adapter, a male cartridge integrated with four drug reservoirs, a thermally expandable layer and microheaters as thermally actuated pumps. b, Concept of plug-n-play microfluidic assembly and disassembly between a female adapter optofluidic probe and a replaceable male drug cartridge that can provide long-term, repeated drug delivery (left) and their respective cross-sectional optical images highlighting the ‘plug-in’ interaction at the plug-n-play interface (right). c–f, Optical images that illustrate device assembly. c, A replaceable male cartridge loaded with red fluid. The inset shows a side view of the replaceable male cartridge after activating one of its chambers with a smartphone, showing ejected fluid at the tip of a male cartridge pillar. d, A female adapter microfluidic probe plugged into the replaceable male cartridge for microfluidic assembly. e, An optofluidic probe system consisting of a microfluidic probe integrated with μ-ILEDs for simultaneous fluid delivery and photostimulation. f, An optofluidic probe system demonstrating its capability for simultaneous and independent control of blue and orange μ-ILEDs. The insets highlight flexible nature of the optofluidic probe that can provide selective, independent control of μ-ILEDs. g, Schematic illustration of a concept of chronic wireless pharmacology and optogenetics using an optofluidic device with replaceable drug cartridges. After delivering fluids (left), the used drug cartridge can be replaced with a new one via plug-n-play disassembly and assembly (middle) for repeated fluid delivery (right). This replaceable cartridge enables chronic delivery of distinct or same fluid. Integrated with an optofluidic probe, the device offers simultaneous and independent control of fluid and light delivery for long-term neural intervention (right). h, Cross-sectional view of a plug-n-play optofluidic system assembled with a replaceable drug cartridge (i), an ultrathin, soft optofluidic probe integrated with the female adapter connected to four microfluidic channels (ii), Bluetooth wireless control module (iii) and two rechargeable lithium polymer batteries (iv). i, Optical image of a freely moving mouse implanted with a wireless plug-n-play optofluidic system. j, A series of optical images showing multiple sequential wireless fluid delivery in a brain tissue phantom (0.6% agarose gel) using three different replaceable drug cartridges with green (i), red (ii) and blue (iii) dye aqueous solution.
Figure 1g illustrates a concept of device operation with replaceable drug cartridges for chronic wireless in vivo pharmacology and optogenetics. After delivering fluid to the target site in the brain, the drug supply can be easily renewed by simply ‘unplugging’ the male cartridge from the implanted female adapter optofluidic probe and ‘plugging in’ a new one (Fig. 1g, middle). The harness that securely holds the cartridge provides another means to guarantee robust microfluidic assembly between the optofluidic probe part and the drug cartridges. With this replaceable cartridge concept, the drug reservoirs can be replaced as often as needed, while the soft implanted probe stays intact to provide independent or simultaneous delivery of multiple, distinct drugs and different wavelengths of light (blue or orange) to the same brain region of interest (Supplementary Fig. 1–2). This design makes the optofluidic probes reusable for unlimited, repeated drug delivery, and also minimizes brain tissue damage that would otherwise be worsened by multiple, disruptive surgeries required to implant new devices. Its construction allows the delivery of two or more distinct drugs simultaneously or with a high-precision temporal control (Supplementary Fig. 3, Supplementary Video 1) for a customized, combinatorial in vivo pharmacology approach. Figure 1h shows the cross-sectional schematic of a fully self-contained, wireless plug-n-play optofluidic system, highlighting the key components (Supplementary Fig. 4); (1) a male replaceable drug cartridge, (2) a female adapter optofluidic probe, (3) a BLE wireless control module on a flexible printed circuit board (Supplementary Fig. 5) and (4) two rechargeable lithium polymer batteries. The standalone wireless system assembled into a three-dimensional (3D) printed case is small (1,260 mm3) and lightweight (~2 g; Supplementary Fig. 4b), and therefore does not obstruct animals’ natural movement and behaviour (Fig. 1i and Supplementary Fig. 6). The proof-of-principle experiment with a brain phantom (0.6% agarose gel) and multiple fluid releases into solution (water) proves that the wireless optofluidic system can make reliable, multiple deliveries of distinct or the same fluid with the simple replacement of drug cartridges (Fig. 1j and Supplementary Video 2). This attribute, combined with programmability for fluid and LED control, supports the notion that the wireless plug-n-play optofluidic system is useful for chronic, versatile neuroscience studies in freely behaving animals.
Thermal, fluidic and mechanical characteristics of wireless plug-n-play optofluidic neural implants
The optofluidic system uses thermally actuated pumps for drug delivery. Figure 2a illustrates the operational principle of the fluidic pumping. Following receiving an activation signal (at t = 0 s) from the wireless transmitter (that is, the smartphone), an electrical current begins to flow through a heater (resistance ~125 Ω), resulting in a localized temperature increase by Joule heating until the current stops after t = 20 s (Fig. 2b). When the temperature rises above the threshold of ~ 82 °C (ref. 8), it leads to an irreversible volume expansion of the polymer composite layer, thereby pumping out fluid from the reservoir through the hermetically sealed plug-n-play interface into the microfluidic probe for ejection. The thermally actuated pump starts to eject fluid from the tip at ~4.5 s and delivers ~93% of the total infused volume in about 12 s (Fig. 2c,d). The device shows minimal variability in the delivered fluid volume (~0.47 ± 0.02 μl) between different reservoirs of the same cartridge, as well as between different cartridges (Supplementary Fig. 7). This reliable, uniform delivery of fluid volume is facilitated by the harness, which robustly joins the plug-n-play interfaces between the microfluidic channels and the cartridge. During actuation, the temperature of fluid in the reservoirs stays below ~60 °C and decays rapidly (within ~0.02 s at the maximum flow rate of 0.87 m s–1) to the ambient temperature around the implanted probe as it comes out through the long (10 mm) and narrow microfluidic channel (with a cross-section of 10 µm × 10 µm), thereby ensuring thermal compatibility with many pharmacological agents and biological tissue (Supplementary Fig. 8; Supplementary Video 3). It is also important for an actuation system to provide moderate fluid pressure during fluid delivery to prevent unwanted neural tissue damage by infused fluid. The finite element analysis (FEA) simulation shown in Fig. 2e,f highlights the spatiotemporal characteristics of the mechanical stress developed during fluid delivery near the microfluidic outlet embedded in brain tissue. The results reveal that even the peak stress developed in tissue during fluid delivery is extremely low (peak stress of 0.77 kPa at t = 8.2 s, which is equivalent to 77 nN force for a 10 µm × 10 µm microfluidic outlet), verifying its negligible influence on brain tissue surrounding the infusion site. While it is possible that fluid delivery itself may modulate neural activity (for example, activation of mechano-receptors), the extremely low pressure exerted from our devices (0.77 kPa), combined with no discernable effects of inert vehicle injections on behaviour, suggest that is unlikely to be the case, at least within the brain sites tested during in vivo studies.
a, Schematic diagram illustrating the mechanism of fluid delivery using a thermally actuated pump. Joule heating of a microheater leads to thermal expansion of an expandable polymer composite into the fluid reservoir, thereby pushing out the fluid through a microfluidic probe. b, Time sequence of infrared images of a heater showing the temperature rise and thermal spread as the activation command is sent from a smartphone at t = 0 s and photographed at t = 1 s (top left), t = 7 s (top right), t = 12 s (bottom left), t = 20 s (bottom right). The white dashed circles represent the location of each of the four pillars and their corresponding reservoirs. c, Time sequence of optical images showing fluid ejection from an optofluidic probe in water as the activation command is sent from a smartphone at t = 0 s and photographed at t = 4 s (top left), t = 7 s (top right), t = 10 s (bottom left), t = 12 s (bottom right). d, Delivered fluid volume as a function of time after actuation of a pump at t = 0 s. e, FEA result showing temporal variation of fluid pressure against brain tissue at the probe–tissue interface during fluid delivery. f, FEA modelling of fluid pressure distribution at the probe–tissue interface at the maximum flow rate during fluid delivery. The maximum pressure applied to tissue is only about 800 Pa, ensuring negligible influence of fluid ejection on tissue. g, FEA simulation of plug-n-play assembly that shows the maximum principal strain (ε) experienced on the inner walls of the female adapter structure by the replaceable male cartridge. The inset shows mechanical pressure generated at the plug-n-play interface due to the assembly. h, The maximum forces required for assembly and disassembly of the plug-n-play parts as a function of plug-n-play insertion length for the PDMS-based female adapter (elastomer: curing agent = 5:1) with a diameter of 1.15 mm and the COP-based male cartridge with a pillar diameter of 1.3 mm. In contrast to the yellow region, the orange region highlights that the force required for assembly and disassembly saturates to peak values at an insertion length greater than 1.5 mm. i, Comparison of the critical pressure required for fluid leakage through the assembled plug-n-play structure and the pressure generated at the reservoir outlet during fluid delivery. The maximum fluid pressure (0.38 kPa) generated at the plug-n-play interface is significantly smaller than the critical pressure for fluid leakage (4,270 kPa), indicating robust, leakage-free plug-n-play microfluidic assembly.
Optimized design of the plug-n-play structures is critically important for robust microfluidic assembly and leakage-free operation. The male pillars (COP) in the drug cartridge are designed to have a slightly larger diameter than the female adapter holes (PDMS) in the probe part (male cartridge pillars OD: 1.3 mm versus female adapter ID: 1.15 mm). Because the modulus of the male cartridge pillars (2.6 GPa) is much larger than the modulus of the elastomeric female structure (~1 MPa), when press-fitted, the female structure experiences large deformation (maximum strain of 52.6%) and exerts radial pressure (~242 kPa) that tightly locks the plug-n-play assembly for hermetic sealing (Fig. 2g). The dimensions of male and female adapter structures are determined by systematic parametric studies to enable robust plug-n-play assembly (Supplementary Figs. 9–10). In our experiments, the maximum force required for plug-n-play assembly and disassembly increases on increasing the insertion length (saturating to peak values at an insertion length ~1.5 mm, Fig. 2h), decreasing female adapter diameters and decreasing PDMS elastomer:curing agent ratio. Our plug-n-play design with optimized parameters (that is, female adapter: hole ID = 1.15 mm, hole height = 1.5 mm, PDMS elastomer:curing agent = 5:1; male cartridge: pillar OD = 1.3 mm, pillar height = 1.7 mm) ensures that the required force for plug-n-play operation is neither too high (inconvenient for in vivo experiments) nor too low (poor hermeticity of plug-n-play assembly). This design also guarantees secure hermetic sealing at the plug-n-play interface such that the maximum fluid pressure developed at the plug-n-play interface (0.38 kPa) is far below the critical leaking pressure (4,270 kPa) (Fig. 2i), thus allowing leakage-free fluid delivery (detailed analysis available in the Supplementary Information). Overall, the device works reliably, such that it delivers desired fluids only when the micro-pumps are activated—that is, changes of the ambient temperature (between 10 and 40 °C) and pressure (between 970 and 1,050 mbar) or plug-n-play assembly/disassembly process do not cause unwanted infusions of fluid (Supplementary Fig. 11–12). During the disassembly of a plug-n-play cartridge, we observed the momentary suction of a minute amount of fluid into the microfluidic channels due to a decrease in pressure inside the channels. However, on plugging in a new cartridge (to replenish drugs) or a blocker (to protect exposed channels in between experiments), the imbibed fluid was pushed back from the microfluidic channels (Supplementary Fig. 12b). Even though the imbibed fluid never travels all the way up to the microfluidic channels, as validated through repeated studies, as a safety measure, the cartridge can be hermetically sealed by transfer-printed copper membranes, which can be ruptured to allow fluid delivery during pump actuation (Supplementary Fig. 13). With this modification, the device will be completely free from unwanted injection or suction.
Smartphone control of wireless plug-n-play optofluidic systems
Wireless manipulation of plug-n-play optofluidic systems is enabled through smartphone control using BLE technology. Figure 3a shows a conceptual illustration of smartphone control (master) of a target mouse implanted with a plug-n-play optofluidic device (target) within the BLE ecosystem, offering easy wireless access, accurate target selectivity and programmable output multi-modality (that is, drug delivery and/or photostimulation). A custom smartphone app (Fig. 3b) facilitates user-friendly control of a target device by allowing easy long-range access to a specific device among many available devices in the vicinity (10–100 m)26 via Bluetooth pairing between a smartphone and the target device (a detailed illustration of the pairing process is available in Supplementary Fig. 14). Through the smartphone app, the user can determine operation conditions of LEDs and heaters (for example, selection of blue and/or orange LEDs, LED modulation frequency, targeted heater number and so on) for independent or simultaneous control of photostimulation and drug delivery (Supplementary Video 4).
a, A schematic of a smartphone Bluetooth control of a specific mouse in a group of multiple mice implanted with wireless optofluidic devices. Bluetooth enables simultaneous and/or independent manipulation of specific outputs (that is single or multiple LEDs and/or one of heaters) for photostimulation and/or drug delivery. b, Screen captures of the smartphone app: Left, the mouse selection panel displaying a selected mouse (Mouse 1) among the list of available mice in the vicinity of the smartphone; middle, the LED control panel with command ‘LED 1 at 20 Hz’ selected (default pulse width: 10 ms); right, the heater control panel with ‘Heater 1’ selected for drug delivery from the reservoir 1. Heater buttons lose their colour (by turning white) if the command is selected at present or has been already sent in the past (a security lock to prevent the user from actuating the same cartridge reservoir twice). Note that two commands can be sent separately or simultaneously. Also, different frequencies can be set for each LED in simultaneous operation mode. c, Optical images of model rats demonstrating Bluetooth selective control capability that can target a specific animal in a group of multiple animals implanted with wireless devices. White arrowheads show illuminated LEDs on different model rats in the right and left panels. Moreover, the target animal can be switched easily with a simple button press on the smartphone app. d, Demonstration of through-wall control of a Bluetooth wireless device: LED 1 (blue μ-ILED, left) and LED2 (orange μ-ILED, right) blinking at 40 Hz. Insets show the zoomed-in pictures of the controlled model rat. e, Optical images highlighting selective control capability of the Bluetooth wireless system implanted in a group of model rats, overcoming the line-of-sight handicap, as well as the limited coverage present in other contemporary wireless technologies, such as infrared and radio frequency. Each coloured line represents a 1 m equivalent separation between the smartphone and each model rat. f, Closed-loop control for a typical place preference experiment, which can be versatilely switched between self-triggered, automated closed-loop control (left) and direct smartphone control (right) modes by simply switching the voltage on a general purpose input/output (GPIO) pin of the SimbleeCOM transmitter.
Although BLE itself is not a new type of wireless technology, its integration with neural devices enables a whole host of possible wireless in vivo neuroscience experiments that have been inefficient and hard to achieve through tethered and other wireless approaches. BLE wireless controls have several compelling advantages for neuroscience experiments over other wireless technologies, such as IR8,9,10,11 and RF12,13,14,15,16,17,18,19,20,21,22,23,24. Unlike IR or other RF systems, BLE provides orientation-independent wireless control, thus guaranteeing reliable omnidirectional activation of a target device, as proven with model rats at various angular orientations (Supplementary Fig. 15a). This feature ensures stable operation of wireless devices in freely moving animals. It also allows a secure wireless binding (pairing) between a smartphone and a selected wireless device for direct control of a target with 100% accuracy, even in a crowded group of animals (Fig. 3c). This opens up new opportunities for complex social behaviour experiments. In addition, unlike IR systems where obstacles can completely incapacitate the wireless control, BLE offers high penetration power of signals through various materials like wood, glass, plastic (Supplementary Table 2) or even walls, without affecting the precision of wireless communication, as demonstrated by the through-door control of a wireless device (Fig. 3d). Moreover, it provides a large range of wireless operation (up to ~100 m)26 without any line-of-sight handicap (Fig. 3e). Other powerful features of the BLE include over the air (OTA) programmability that allows the user to wirelessly reprogram the BLE chip to enable easier adjustment of device operation parameters for various applications, including in vivo pharmacology with high-precision temporal control of multiple fluid deliveries (Supplementary Fig. 3) and closed-loop control for advanced behaviour experiments, as demonstrated in our real-time place preference control experiment. The latter exploits a BLE wireless transmitter (SimbleeCOM protocol27) communicating with a camera tracking system for automated conditional controls, which can be easily switched to the direct smartphone control mode, depending on the application (Fig. 3f). The closed-loop protocol can be further extended to enable complex social behaviour experiments where the behaviour of one animal affects the stimulation parameters of other animals (via positive or negative feedback loops) in the vicinity (Supplementary Fig. 15b and Supplementary Video 5). Another feature of the BLE closed-loop communication is that it allows the user to check the status of wireless operation. In other words, the wireless control can be not only authenticated through ‘success’ or ‘fail’ toasts for the confirmation of the desired operations, but also tracked through the saved timestamp readings on the smartphone app (Supplementary Fig. 16). This function helps to ensure successful wireless operation and avoid visual cues through indicator LEDs on the device during behavioural studies, which can sometimes affect animals’ behaviour. All these incorporated device attributes make BLE a useful and highly functional option for wireless neural implants.
Chronic, wireless drug delivery with precise temporal control produces repeatable behavioural changes in mice
We first aimed to establish chronic reusability over previous wireless and standalone optofluidic technologies8,14 by expanding on the ‘use-n-throw’ nature of the device. Whereas the previous approaches allowed for a one-time heater activation for drug release, our goal was to utilize the plug-n-play components to allow for multiple activations of drug release across an extended timeframe, enabling more chronic applications of this plug-n-play optofluidic technology. Previous work has shown that these types of microfluidic probes have reduced immunoreactive glial responses in comparison to conventional cannulas; however, it is not known whether the immunoreactive glial response changes over time with chronic implantation of these microfluidic probes. To determine the immunoreactive glial responses from chronic, deep brain implantation of these microfluidic probes, we examined astrocytic glial fibrillary acidic protein (GFAP) activity and ionized-binding molecule 1 (Iba1) microglial immunostaining at multiple time points after device implantation (Fig. 4a–c). We observed an initial increase in Iba1 immunoreactivity surrounding the implant one week following implantation, but low expression of GFAP. By week four, Iba1 immunoreactivity reduced substantially, whereas GFAP increased (probably indictive of a glial scar). These results are typical neural responses for an implanted device, similar to cannulated immune responses. However, it is worth noting that the overall area of affected tissue is considerably less with our device than with cannulas. In the images shown in Fig. 4a–c, the device caused a ~100 μm x 400 μm lesion, with a total area of 0.04 mm2. A typical cannula has a radius of ~200 μm, making its lesion area 0.126 mm2. Thus, while our device may cause similar immune responses to traditional approaches, the total area perturbed is only one-third that of a cannula. These results suggest that these microfluidic probes are suitable for long-term implantation, elicit expected glial response over time and do so while reducing overall tissue damage.
Wireless delivery of multiple DAMGO infusions into the ventral tegmental area produces consistent, repeatable increases in stereotypical rotational behavior. a–c, Representative fluorescence images (20×) of 30 µm horizontal striatal slices depicting immunohistochemical lesion staining for activated microglia (a, Iba1, green), astrocytes (b, GFAP, red) and overlaid images either 1 week (left column), 2 weeks (middle column), or 4 weeks (right column) after implant surgery (c). All histological and confocal settings were kept consistent across groups. Scale bar, 100 μm. The white dashed line indicates lesioned tissue from the device. Immune responses were tested twice with similar results, each time with a different set of brains and by different investigators. d, Calendar outlining timeline for device implantation and subsequent, repeated (Baseline, Session 1, Session 2 and so on) OFT tests (60 min per test session), with respective representative heat maps of locomotion after Bluetooth, wireless intra-VTA DAMGO release. The cumulative time spent in each part of the open-field is indicated by low (blue) to high (red) colour gradient. e, Contraversive rotations and f, overall locomotion after within-subject, counter-balanced experiments following Bluetooth, wireless intra-VTA infusion of vehicle (baseline), and DAMGO (1 week, 2 weeks, 3 weeks, 4 weeks post-surgery) (n = 7 mice, repeated one-way ANOVA, *P < 0.05, **P < 0.01; F(4,35) = 4.181, P = 0.0072 for contraversive rotations, F(4,30) = 2.916, P = 0.0377 for locomotion; Baseline mean = 10,321 s.e.m. = 1,048; Session 1 mean = 32,431 s.e.m. = 8,177; Session 2 mean = 33,146 s.e.m. = 6,447; Session 3 mean = 30,384 s.e.m. = 5,504; Session 4 mean = 26,204 s.e.m. 3,589). Data represented as mean ± s.e.m. g, Bidirectional behavioural modulation through multidrug infusions in VTA within the same animal cohort (n = 6 mice) using the same devices that were wirelessly reprogrammed with precise temporal delays. DAMGO infusions (red arrow) robustly increased locomotor activity (distance, cm) and velocity (cm s–1, values in red parentheses) compared with vehicle injected mice (dashed yellow line, values derived from Fig. 4e,f). Naloxone infusions occurred 10 (left), 20 (centre) or 30 (right) min after DAMGO in the same mice across different test days (counterbalanced). Naloxone blocked DAMGO enhanced locomotion and velocity (values in blue parentheses). h, A comparative bar graph highlighting the relative decrease in average velocity (cm min–1) when naloxone is released 10, 20 and 30 min after releasing DAMGO (n = 6 mice, repeated one-way ANOVA, *P < 0.05, **P < 0.01; F(1,9) = 41.18, P < 0.001; left, P = 0.041, DAMGO mean = 205.85 s.e.m. = 33.42, Naloxone mean: 106.1 s.e.m. = 16.9; middle, P = 0.008, DAMGO mean = 250.83 s.e.m = 30.65, Naloxone mean: 141.83 s.e.m. = 32.45; right, P = 0.007, DAMGO mean = 195.15 s.e.m. = 78.38, Naloxone mean: 76.11 s.e.m. = 24.53). D, DAMGO; N, naxolone; Ses, session.
To demonstrate the feasibility of chronic, repeated delivery of localized pharmacological agents, we implanted microfluidic devices unilaterally into the ventral tegmental area (VTA) of wild-type mice (C57Bl6). Previous studies have shown that activation of µ-opioid receptors (MOPRs) within the VTA cause a pronounced, rapid increase in locomotion as well as a dramatic increase in stereotypical contraversive (from the site of drug delivery) rotational behaviour28,29, making this an ideal demonstration behaviour for repeated pharmacological challenge in vivo. We then wirelessly delivered the selective MOPR peptide agonist, DAMGO ([D-Ala2, N-MePhe4, Glyol]-enkephalin, 500 pmol, 0.5 µl total volume, Tocris), into the VTA of wild-type mice performing an open-field task (OFT) across multiple timepoints post-surgery (1 week, 2 weeks, 3 weeks and 4 weeks after device implantation) (Fig. 4d). We found that intra-VTA DAMGO significantly increased the number contraversive rotations (Fig. 4e) as well as the distance travelled (Fig. 4f) (locomotor activity) in comparison to baseline measurements. Additionally, DAMGO-induced increases in rotations and locomotor behaviour were consistently maintained at all measurable timepoints (Fig. 4e,f) for up to at least 4 weeks post-implantation (Supplementary Video 6). Although tested for only 4 weeks, the replaceable nature of these devices could allow for long term chronic pharmacological delivery for the duration of the animal’s lifetime (>6 months). It should be noted that activation of only one reservoir was sufficient to produce DAMGO-mediated behavioural effects, and that we used the same microfluidic channel by activating the same location reservoir in a new cartridge throughout the behavioural paradigm. This result strongly suggests that the microfluidic channels remain unobstructed over long-term use or after repeated use. However, it is also feasible to use a separate cartridge filled with saline and activate the same microfluidic channel to flush the channel from the previous use or drug.
To further highlight the wirelessly reprogrammable, temporally controlled capabilities for multiplexed drug deliveries within the same behavioural session, we infused intra-VTA DAMGO, followed by an intra-VTA infusion of the non-selective, competitive opioid antagonist naloxone ((5α)−4,5-Epoxy-3,14-dihydro-17-(2-propenyl)morphinan-6-one hydrochloride) at various timepoints (10, 20 and30 min after DAMGO) (Fig. 4g). We demonstrate that naloxone reverses the DAMGO-induced increases in locomotion in a time-specific manner (Fig. 4g), thereby demonstrating multi-drug release within the same brain region during a single behavioural task. It is worth noting that, DAMGO-increased locomotion remained significantly high until the delivery of naloxone (Fig. 4h). This same animal could feasibly be controlled via multiple drug deliveries over an extended timeframe through replaceable drug cartridges and wirelessly reprogrammed time delays, thus highlighting its precise temporal control for multiplexed drug delivery. Taken together, these proof-of-principle experiments demonstrate that these optofluidic devices are suitable for chronic, repeated delivery of agents with precise temporal control within the deep brain of awake-behaving animals.
Wireless, selective control of drug delivery within a group of simultaneously behaving mice
Another drawback from earlier wireless optofluidic device approaches8,14 was the inability to efficiently activate a specific mouse selectively in a group of multiple mice within a compact laboratory behavioural space. This limited the investigator to running one animal in a behavioural assay in an area well separated from other animals. This is true for most wireless technologies8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24, as requirements for the specific receiver antenna design and unique transmitter setups severely limit the combinatorial scalability and selectivity to efficiently run multiple behavioural experiments within a confined space that consists of different treatment groups with same, or distinct, stimulation parameters. To determine the capability of individual selective control within a group of mice, we implanted wildtype mice (C57/Bl6) with optofluidic devices into the VTA. During the test day, we filled two of the cartridges with vehicle (saline), and the other cartridges with DAMGO. We then placed each animal within an open field arena that was spaced 10 cm from the other open field arenas for a 60 min open field test (Fig. 5a). After the start of the session, we wirelessly delivered either vehicle or DAMGO at different timepoints within the 60 min test session (Fig. 5b). We found that wireless activation of intra-VTA DAMGO at different timepoints within the same session rapidly increased both contraversive rotations and distance travelled, in comparison to mice that received wireless activation of intra-VTA vehicle (Fig. 5c–f, Supplementary Video 7). Additionally, in utilizing a smartphone-based app for selective control, there was negligible temporal lag in the feasibility of switching reservoir activations between individual mice. This was also a clear indication that Bluetooth signal interference did not impact the behaviour of surrounding mice. These data demonstrate the multiplexed capability of these optofluidic devices for dynamic, selective control of pharmacological manipulations in several individual mice concurrently within a behavioural paradigm.
Individual, selective control of wireless-mediated intra-VTA infusion of DAMGO increases stereotypical locomotor behavior within a group of mice. a, Behavioural paradigm depicting colour-coded mice behaving simultaneously in separate, neighbouring (10 cm) arenas that correspond to panels b–f. b, Timeline depicting separate Bluetooth, wireless heater activations of intra-VTA vehicle (Veh) or DAMGO release within multiple mice during the same 60 min OFT test. c,d, Representative heatmaps (c) and traces (d), depicting locomotion from the last 30 min of the OFT session corresponding to panel b. e,f, Locomotion (e) and contraversive rotations (f) during within-session 10 min epochs after separate heater activations of intra-VTA vehicle (Veh) or DAMGO release with colours corresponding to mice in panel b (n = 4). Data represented as within-session total during 10 min time epochs.
Incorporation of wireless photostimulation and wireless pharmacology in awake, behaving mice
We next sought to demonstrate the in vivo capabilities of this plug-n-play optofluidic device by extending the above drug delivery capabilities to incorporate concomitant optogenetics and pharmacology. We chose to demonstrate this multiplexed functionality in a real-time place-preference assay. This close-loop behavioural method is now heavily utilized in behavioural neuroscience to assess the valence of a brain circuit within a neutral context30. It has been previously reported that photostimulation of the bed nucleus of the stria terminalis (BNST) GABAergic terminals in the lateral hypothalamus (LH) promotes reward-like behaviours31. Using this model, we tested whether selective activation of the vGATBNST-LH pathway would produce a specific preference within a neutral context using a real-time place test assay (RTPT). In a RTPT, animals have access to two identical chambers and receive photostimulation on entering one chamber, but not the other (counterbalanced across animals). Here, we employed a closed-loop BLE network (SimbleeCOM protocol), which can be synchronized with an animal tracking camera system in which the animal’s behaviour conditionally triggers activation of the μ-ILED. The SimbleeCOM transmitter was placed outside the chamber and, based on the nature of received interrupts (depending on position of the mouse) from the camera tracking system (Noldus Ethovision), it wirelessly manipulated the device (μ-ILED stimulation) in the animal by sending out pre-configured commands. Preference and avoidance data are then calculated as time spent in the photostimulation-paired chamber, expressed as a percentage of total time32,33. To stimulate this pathway, we first injected a Cre-dependent Channelrhodopsin-2 viral construct (AAV5-DIO-EF1α-ChR2-eYFP) unilaterally into the BNST of vGAT-Cre mice and positioned optofluidic devices in the LH to allow for photostimulation of GABAergic projections (Fig. 6a,b). We then tested animals for three consecutive days consisting first of a 20 min baseline session with no stimulation. This was then followed by a 20 min, 20 Hz session where animals received photostimulation (20 Hz, 10 ms pulse width, 470 nm wavelength) on entering the photostimulation-paired side. Lastly, the animals received micro-infusions of gabazine (GABAA receptor antagonist) into the LH before undergoing the real-time place testing session. In accordance with the previous findings30, we found that vGAT-Cre mice expressing ChR2 exhibited a robust preference for the photostimulation-paired chamber in comparison to their baseline measurements (Fig. 6c). However, wireless pharmacological delivery of gabazine (10 µM, 0.5 µl total volume, Tocris) into the LH before to the real-time place preference assay completely prevented the preference normally generated by concurrent 20 Hz photostimulation (Fig. 6d). We found no effect of 20 Hz photostimulation, nor gabazine + 20 Hz photostimulation on locomotor activity, compared with the baseline, during the real-time place preference test sessions (Fig. 6e). These data demonstrate the parallel incorporation of smartphone, wireless control of µ-ILED photostimulation of neural circuits in combination with pharmacological delivery in freely moving mice.
Wireless activation of gabazine blocks vGATBNST-LH photostimulation-mediated real-time place preference. a, Schematic diagram of ChR2 virus injection into the BNST and optofluidic device implantation into the LH. b, Coronal images (40×) of ChR2-eYFP terminal expression in the LH following viral injection in vGAT-Cre animals. Images show Nissl (blue) and ChR2-eYFP (green). EP, entopeduncular nucleus; f, fornix; 3 V, third ventricle. Placements and viral expression were verified for each mouse tested. c, Subsequent panels depict 20 min RTPP sessions with corresponding, representative heat maps of locomotion during baseline, 20 Hz photostimulation, and 20 Hz photostimulation with gabazine sessions. d, Photostimulation of BNST-LHGABAergic terminals (473 nm, 20 Hz, 10 ms pulse width) expressing ChR2 drives a real-time place preference, as measured by the percentage of time spent in stimulation side, and is blocked by pre-session infusion of gabazine. Shaded zones indicate separate test days: white, vehicle infusion; light blue, 20-Hz stimulation; dark blue, 20-Hz stimulation with gabazine pretreatment. All data represented as mean ± s.e.m. (n = 6 mice one-way ANOVA, **P < 0.01; F(6,12) = 9.702, P = 0.0062; Baseline mean = 49.98 s.e.m. = 2.53; 20 Hz mean = 72.10 s.e.m. = 5.91; gabazine mean = 52.80 s.e.m. = 2.33). e, Total locomotion was not different across all session of RTPP testing (n = 6 mice one-way ANOVA, F(6,12) = 1.257, P = 0.3456; Baseline mean = 2803 s.e.m. = 624; 20 Hz = 1,785 s.e.m. = 348; gabazine mean = 2,452 s.e.m. = 340).
Discussion
We have described the development of a combinatorial wireless device approach for in vivo neuropharmacology and optogenetics that is a self-contained multifunctional system capable of chronic, selective control within freely moving animals. These thin, flexible neural probes allow researchers long-term, biocompatible optofluidic access to neural tissue deep inside the brain as well as chronic drug supply with temporal control through its replaceable plug-n-play drug cartridges. The approach provides scalable output modalities with programmable wireless control where an easy-to-use smartphone app transforms any commercial smartphone into a long range and isotropic wireless transmitter possessing wireless reprogrammability, as well as precise selectivity within large animal cohorts. This provides an important advancement from the existing embodiments of fluidic neural interfaces6,7,8,14,34,35,36 (Supplementary Table 1).
When compared with the smallest commercial alternatives (SMP-300, iPrecio; Supplementary Table 3), it offers greater in vivo capabilities by allowing multidrug release without disrupting an animal’s natural behaviour in a single behaviour session. The device also allows for easy switching of drugs through replaceable plug-n-play cartridges for versatile chronic studies, a feature not available with the commercial wireless pump. These commercial pumps can deliver only a single drug within a behavioural session and require a cumbersome process of cleaning a reservoir before replacing the original drug with a different type. Their chronic utility is further limited by their disposable nature, lasting only 1–8 weeks due to limited battery life. Furthermore, our device presented here is smaller and lighter (ours: 1,260 mm3; 2 g versus SMP-300: 2,678 mm3; 3.3 g) and allows programmable and combinatorial neural manipulation with four distinct drugs and two wavelengths of light. Thus, its ultra-compact footprint with multimodal features allows implantation in freely moving animals as small as mice. However, the plug-n-play device is limited due to its head-mounted configuration and lack of ability to control flow rate and deliver a large volume of fluid at once, which can be provided by commercial pumps in a fully implantable design (Optofluidic: 0.5 µl per delivery versus SMP-300: variable volume up to 130 µl per delivery). However, it must be noted that the volumes delivered by the plug-n-play device (0.5–2 µl) using replaceable cartridges are more practical for experiments looking at the role of specific neurochemical systems and also more feasible for chemicals that can either degrade, or are not able to maintain their quality if stored at body temperatures (as in implantable commercial pumps like SMP-300) for several months. Due to their own advantages and disadvantages, we believe the plug-n-play optofluidic device and commercial pumps can offer unique solutions to various applications in a complementary way. For example, the plug-n-play optofluidic device would be more suitable for neuroscience research applications, which require chronic delivery of both drug and light, highly localized drug delivery for dissection of neural circuitry, and multiplexed delivery of multiple, distinct drugs for advanced pharmacological studies. On the other hand, commercial wireless pumps such as SMP-300 are viable in studies that involve delivering large amounts of single drug over long periods of time with precise flow control. Moreover, their fully implantable nature has the potential to extend their use to clinical applications.
Current features of the plug-n-play device have the ability to minimize the stress imposed on the surrounding brain tissue normally associated with conventional rigid drug delivery cannulas, and also the behavioural stress imposed on the animal associated with tethering4,5. The miniature and mechanically compliant nature of the optofluidic probes improve its chronic in vivo integration by reducing the glial response and tissue inflammation that occur during surgical implantation, as well as due to micromotions within surrounding soft neural tissues post-surgery. In contrast, the rigidity in conventional metal cannulas causes lesions and deleterious tissue inflammation that can subsequently lead to cannula clogging after repeated use. For in vivo studies, this adverse effect is further reduced in freely moving animals by untethering soft optofluidic probes through integration with a wireless technology. This allows for minimal disruption to the natural state of the animal as well as uninterrupted access during ongoing behaviour when employing multiple infusions of a drug compound during a behavioural session. This wireless capability also enables researchers to trigger untethered animals from outside the behavioural room (up to ~10 m through indoor walls, Fig. 3d), or in a preprogrammed manner while they are within a natural environment. Even after improving their mechanical compliance, tethered drug delivery systems6,7,36 still promote either angular stress and higher risk of tissue inflammation on freely moving animals (if tethered throughout session), or dictate that the infusion has to take place before the experiment (if untethered during session). For an in vivo session, the latter means that the animal has to be typically removed from their current, ongoing behavioural environment, thus limiting the real-time manipulation of particular cellular targets with multiple infusions.
Another key feature of the plug-n-play optofluidic devices is their capacity for chronic wireless drug delivery to the same target region of brain. In the previous systems8,14, to deliver pharmacological compounds more than once, an integrated drug reservoir with four individual chambers was used to deliver four similar or different drugs, allowing multiplexity within the same localized region. But this severely limited such devices for chronic studies, as they were completely unusable after all chambers were activated due to the irreversible expansion of the thermally expandable polymer actuators. By implementing a detachable plug-n-play interface (Fig. 1b), the plug-n-play device allows for repeated, unlimited and chronic pharmacological manipulation within an untethered, freely moving animal, demonstrating a substantial improvement over the previous optofluidic remote-delivery systems8,14. This feature was highlighted by recurring intra-VTA DAMGO unilateral infusions (Fig. 4) in live mice where we observed consistent, repeated increases in stereotypical locomotion up to at least a month after implantation of the optofluidic device. The head-mounted non-removable part of the implant is robust enough to last several months (>six months), with the addition of Metabond (see Methods), and therefore, in principle, can allow for in vivo pharmacology for an extended timeframe. Furthermore, we repeatedly delivered pharmacological agents using different drug cartridges through the same microfluidic channel (same heater activation), thus suggesting that the microfluidic channels do not become blocked or clogged over time after repeated use. The cartridge replaceability provides the option to change or refill drug compounds (Supplementary Fig. 17–18) within the same, or different, behavioural session, and also overcomes the evaporation issue that presents in previous wireless devices8,14; where limited non-chronic drug sources must be delivered within 2 weeks after surgical implantation, thus significantly shortening their experimental timeline. In addition, its ability for precisely controlled temporal delivery of two or more similar or distinct drugs within a single experimental session opens avenues for versatile, combinatorial chronic pharmacology in freely moving animals. Such chronic and combinatorial, yet localized, pharmacological intervention of neural circuits with precise temporal control is rare, and enables researchers to test compounds in pre-clinical phases through long-term repeated in vivo drug deliveries at the same target location. This is an improvement over other non-localized pharmacological methods such as oral delivery, topical application or intravenous injections, which can be slow-acting and may also lead to off-target exposure or rejection through the blood–brain barrier, thus adversely affecting their selectivity, efficiency and reliability. From just a single surgical implantation, (Supplementary Fig. 19), this miniaturized device can provide high spatio-temporal and multi-modal access to a target neural circuit in a series of experimental testing. The ability to deliver viral vectors and pharmacological agents, as well as light locally over long epochs of time, could also enable chronic optopharmacological studies in the future. In turn, the full capability of this device could decrease the need for experimental subjects, as well as the experimental timelines. The ability to chronically administer drugs to a highly localized region in a non-tethered nature offered by this approach could also have future implications in boosting advancements in repeatable targeted chemotherapeutics.
One of the main advantages of this wireless plug-n-play device is its ability to transform any commercially available smartphone into a custom wireless transmitter with a long omnidirectional range (up to ~100 m), through an easy-to-use and readily available smartphone app. This eliminates not only the need for special transmitter electronic systems and/or bulky control equipments8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24, including special resonant cavities17,24 or special antenna cages16,20; but also the requirement to modify behavioural apparatuses to conform with wireless integration. Therefore, this smartphone-based wireless technology allows a researcher to simply test the animal in any of their existing behavioural paradigms. Moreover, simple keystrokes on the readily usable app and easily customizable smartphone control parameters (Fig. 3b) enable smooth and ‘on-the-fly’ rapid transitions between optical and pharmacological modalities. Another advantage of the plug-n-play optofluidic device is the ability to selectively control specific mice during a single behavioural session within a limited, confined space (Fig. 5). One limiting feature of many recent wireless techniques involving optogenetic or pharmacological control8,9,10,11,12,13,14,15,16,17,21,23,24 is their lack of capacity for versatile selectivity (for both animal selection and configuring its multimodal output) that is scalable, although some of such systems can allow selectivity to a certain degree by modifying their hardware or transmitter setups. This is further limited by the wireless equipment size and laboratory spaces, which can hinder their configurability for versatile and on-the-fly selection of target animals and/or output modes (light or drugs) with variability in stimulation parameters. By harnessing software intelligence integrated within its hardware, the plug-n-play device overcomes such limitations by allowing not only accurate specificity of animal selection within a large congested group, but also scalability and programmability of multimodal outputs within each selected animal. This allows researchers to trigger each animal in a large group using its own distinct stimulation modes and parameters, without modifying receiver hardware or requiring special transmitters and set-ups. This can also overcome the singular paradigm nature of behavioural experiments within limited laboratory spaces. Running multiple animals within the same congested behavioural cage can help increase data generation and research efficiency without significant modification of a laboratory environment. The ability to test multiple mice during a behavioural session is critical for productivity, high throughput, and behavioural consistency (that is timing of day, room temperature and so on). Other key advantages of the Bluetooth technology include wireless reprogrammability, which can allow researchers to change stimulation parameters on the fly. Moreover, the system offers not only easy to set up and scalable closed loop systems, enabling social experiments with dependent feedback-based triggering (Supplementary Video 5), but also obstacle invariability, permitting researchers to initiate actions from outside the behavioural room, using a simple smart phone graphical user interface (UI).
The device materials and design are devised to be rapidly reproduced in most engineering labs with access to basic tools. Many of the components of the device (Supplementary Fig. 4) are either readily available (electronic components, rechargeable batteries, connectors and so on), 3D printable (case, case covers, harness, male cartridge and so on), or can be fabricated with a simple soft lithography in a standard fabrication laboratory (female adapter optofluidic probe). Researchers with basic training can easily fabricate and assemble a multitude of optofluidic probes within a few days. The economical overheads can be further reduced through reusing these devices (Supplementary Fig. 20) by finding a technique to cleanly eliminate the dental cement or adhesive used to attach the optofluidic device to the skull, without damaging the devices. Moreover, the stackable nature of this probe architecture12 allows versatile functional scalability by integrating multimodal components, such as pressure, temperature and chemical sensors, as well as recording electrodes. Such attributes can reduce costs and time to prepare, and allow more complex neuroscience experiments.
Integration of advanced materials and efforts for optimized engineering design can help to unleash the full potential of this device by further improvements and fully recognizing its current limitations. Currently, the inability to easily modify the volume of fluid delivery and the infusion rate hinders the real-time customization of fluid control, limiting some applications. However, we can deliver the same type of fluid to the target neural circuit multiple times to compensate for the required dose deliveries. Alternatively, the dose amount and flow rate can be controlled by modifying the reservoirs and microfluidic channel dimensions in a similar design architecture, or can be fully overcome by integrating microstepper motors or micromachined linear actuators for refined fluid control. The current thermal actuation technique also requires the drugs to be thermally stable and compatible with the reservoir temperatures (~60 °C) during the very brief heater activation. The concern associated with high temperature actuation can be dramatically mitigated by replacing the current expandable polymer composite with thermally responsive hydrogel, which can be engineered to have an activation temperature as low as 32 °C (refs. 37,38). The use of hydrogel, which is intrinsically hydrophilic, in drug reservoirs can also facilitate loading drugs into cartridge reservoirs, thus eliminating the need for oxygen plasma or ozone tools for hydrophilic treatment, which are not readily accessible to neuroscientists. Additionally, although mice tolerate these head-mounted devices well, the device can be potentially damaged or detached from the head by very active movements or social defeat interactions. This also limits their ability to access various space-critical locations within the peripheral nervous system, unlike fully implantable devices where an entire system can be implanted under the skin14,15,16. Besides, the current head-mounted wireless module design requires a somewhat cumbersome assembly and disassembly process for battery recharging (Supplementary Fig. 18), although it can be further optimized to some extent by using magnetic plug-n-play connectors for quick swapping of fully charged batteries to save time and effort. All these issues associated with the head-mounted design could be possibly resolved by creating miniaturized, wireless neural systems that could be chronically embedded in tissue. Combinatorial integration of custom-fabricated or unpackaged Bluetooth and application-specific integrated circuit (ASIC) chips, wireless energy harvester and drug reservoirs refillable with a syringe needle from outside the skin has the potential to create such systems. Specifically, this fully implantable device could be achieved by encapsulating the entire system with soft, biocompatible waterproof structures39. Moreover, integration of Bluetooth-based neural devices with Internet networks (for example, Wireless Fidelity (WiFi)) can open avenues for simultaneous, large scale triggering of remote animals in a highly programmed throughput manner. These large networks can also allow for simultaneous selective control of multiple animals, each with a different command (treatment) in the same behavioural space, thus aggrandizing experimental throughput and efficiency, enabling quick and reliable acquisition of large data sets and hence permitting faster experimental timelines. Integrating such technology with the Internet can help transfer data by exploiting the high throughput capabilities of WiFi as well. Utilizing the processing power and software tools in smartphones, along with programmable capabilities of BLE modules, experiments can also be programmed to deliver drugs or trigger photostimulation during a specific time of day and thus can considerably reduce the experimental burden for circadian-sensitive experiments. This will allow neuroscientists to run automated, pre-defined, programmable and high throughput animal studies without always being present in their laboratories. Finally, it is important to acknowledge that our device still elicits typical immune responses from the implantation process, similar to other implantable tools, such as stainless steel cannulas. While future iterations of the device may further enhance its biocompatibility, the use of soft polymeric material produces substantially less damage, lesioning two-thirds less tissue than a functionally comparable cannula. Additionally, our device only damages 0.002 mm2 more tissue than an optic fiber (diameter ~0.22 mm), which is presently one of the smallest implants used in neuroscience research. Thus, our device is able to perform two distinct experimental capabilities (pharmacology and optogenetic stimulation) without increasing neural tissue disruptions more than traditional cannulations or modern optic fibres, both of which can only perform one function.
We have presented a wireless plug-n-play optofluidic technology that provides technology for chronic behavioural studies involving in vivo pharmacology and optogenetics. This approach allows researchers the ability to selectively control single or multiple animals within a congested vicinity with an easy to use Bluetooth smartphone app. The potential of these devices will be greatly enhanced as the field of in vivo photopharmacology advances40,41,42, where photosensitive compounds can modify protein activity on exposure to certain wavelengths of light. This technology enables compound control using optofluidics in a variety of experimental settings, and allows for naturalistic animal behaviours and chronic in vivo studies.
Methods
Fabrication of a female adapter optofluidic probe
The three distinct layers of the ultrathin, soft female adapter optofluidic probes (the female adapter layer, the microfluidic probe layer and the optical probe layer) were fabricated through soft lithographic and photolithographic techniques. For the female adapter, a mould (70 mm × 45 mm) consisting of a 3 × 5 array of female adapter structures was printed by a 3D printer (Objet30, Stratasys). Degassed 5:1 PDMS (base: curing agent) was cast into the mold, followed by pressing and clamping with a polycarbonate (PC) sheet supported by a glass slide (75 mm × 50 mm). After curing at 70 °C in oven (for about 70 min), the PC sheet and the glass support were delaminated, and the 3 × 5 female adapter array was removed from the mold surface. The 1.5 mm thick array was then cut into individual female adapters (10 mm × 7.5 mm) along the alignment marks under an optical microscope (OM4713, Omano). The mould was washed with isopropyl alcohol (IPA) and let dry at room temperature (~1 day) or in an oven (70 °C for ~1 h) before pouring PDMS again and reusing in another batch. A puncher (1.2 mm ID, Harris uni-core) was used to cut clean through-holes (1.15 mm) in the female adapter layer. The microfluidic probe layer, consisting of four parallel ultrathin, soft microfluidic channels (10 μm × 10 μm × 10 mm), was fabricated through soft lithography using 10:1 PDMS as outlined in our previous work8,9. The channel inlets of the microfluidic layer were aligned and connected to the female adapter holes using a double-sided silicone adhesive (ARClear 8932EE) under a stereo microscope. The microfluidic connections through the female adapter holes were then manually tested by pushing deionized water through a blunt syringe needle (18 Gauge), plugged into the female adapter hole (1.15 mm ID). The optical probe layer was prepared using a similar process presented in our previous studies8,12,13. After creating metal electrodes (5 nm/250 nm of Cr/Au) on a 6μm thick PET film, two μ-ILEDs—blue (470 nm, TR2227, Cree Incorporated) and orange (589 nm, TCE10–589, Three Five Materials) were attached to their respective electrodes using a silver epoxy (Cat. No. 8331, MG Chemicals). An anisotropic conductive film was bonded to the optical probe. The optical probes were then coated with 7-μm-thick Parylene C using a PDS 2010 Labcoater 2 (Specialty Coating Systems) to insulate the μ-ILEDs and metal electrodes from the biofluid for in vivo experiment. After confirming the functionality of both the microfluidic (with female adapter) and optical layers, the two layers were attached together using double-sided silicone adhesive (ARClear 8932EE) to form the female adapter optofluidic probe (Fig. 1a,b). Further fabrication details can be found in the Supplementary Information.
Preparation of replaceable male drug cartridges
The plug-n-play drug reservoirs with four (2 × 2 array with 3.1 mm pitch) male cartridge pillars (1.7 mm long, 1.3 mm OD) were machined from a 3 mm thick block of cyclic olefin polymer (COP, Zeonor 1420 R) with low water permeability (0.028 g mm m–2 day–1). Thermal actuators for pumping drug out from reservoirs were created with Cr/Au (5 nm/250 nm) serpentine traces on a FR-4 substrate covered with a thermally expandable polymer composite on top8,9,14. The male drug cartridge reservoirs were then attached on the thermal actuators using a double-sided adhesive (ARClear 8932EE) after aligning each of its four reservoirs to the four microheaters. A 7-μm-thick Parylene C was also coated on the inner walls of the reservoirs and pillars (PDS 2010 Labcoater 2, Speciality Coating Systems) to further minimize drug evaporation. To facilitate drug loading into the hydrophobic reservoirs, they were made temporarily hydrophilic through oxygen plasma treatment (300 mtorr/200 W/55 s/6 sccm O2 in March Jupiter III RIE), and desired drugs were then loaded using thin blunt syringe needles (30 Gauge, 0.31 mm OD). To minimize drug evaporation from open pillar ends, the pillars were plugged by a Parylene C-coated, 3 mm-thick PDMS (Supplementary Fig. 17) cover consisting of cylindrical cavities (1 mm long, 1 mm ID) for each pillar and kept frozen at −20 °C until ready for the in vivo experiment—the fabrication of PDMS covers followed same procedure as the female adapter layer.
Pressure analysis for drug delivery in the target deep brain tissue
To analyse the spatiotemporal distribution of pressure and stress during drug delivery near the target brain tissue, FEA was carried out to simulate the fluid flow and mechanical stress built up around the brain tissue (COMSOL Multiphysics version 4.2, COMSOL Inc.). The fluid flow was assumed to be laminar with the experimentally measured flow rate (Fig. 2d) and to have fluid properties of a density of 1,000 kg m–3 and a dynamic viscosity of 0.89 Pa ms. Brain tissue was modelled as a poroelastic material with a Young’s modulus of 3,156 Pa, Poisson ratio of 0.35, porosity of 0.3 and compressibility of 0.35 (ref. 43). The PDMS microfluidic probe layer was assumed to be a linear elastic material with a Young’s modulus of 1 MPa, and Poisson ratio of 0.49. For simplicity, we used a two-dimensional cross-sectional model for the brain tissue and fluid flow interaction. The resulting mechanical stress near the target brain tissue was extracted by von Mises stress to display a scalar value of stress from the Cauchy stress tensor (Fig. 2e,f).
Fluid leak analysis at the plug-n-play interface
Mechanical analysis of fluidic leaking between the male drug cartridge and the female adapter optofluidic probe was performed using 3D FEA software (Abaqus, Dassault Systèmes) by simulating the mechanical interaction pressure developed between the assembled plug-n-play parts and a simplified estimation of fluidic flow pressure at the plug-n-play interface. Eight-node, 3D hexahedron elements (C3D8R) were used to model the soft female adapter (E = 2 MPa; each hole with ID = 1.15 mm) and the rigid male cartridge (E = 3 GPa; each pillar with OD = 1.3 mm). Then the deformation and strain distribution in the female component of the plug-n-play assembly was calculated, in order to estimate the critical leaking pressure at the plug-n-play interface44. Based on our measured data for fluid velocity, we analytically estimated the fluidic pressure developed at the plug-n-play interface during fluid delivery, and quantitatively compared this fluidic pressure with the critical leaking pressure to evaluate fluid leaking through the plug-n-play interface. For detailed analysis, please see the Supplementary Information.
Mechanical analysis of plug-n-play assembly and disassembly
Mechanical characterization of the plug-n-play assembly and disassembly processes was carried out using Instron Mechanical Testing System. To align the structures before testing, the female adapter was first glued on top of a glass slide (75 mm × 25 mm), which was fixed to the bottom of the loading clamps of the mechanical testing machine. The male cartridge (each pillar with OD = 1.3 mm) was then assembled into the female adapter, and liquid thermal glue (Mini Hot Melt Glue Gun, CCbetter) was applied on top of the assembly (the opposite surface to the male cartridge pillars). The upper loading clamp of the machine was driven down, attaching it to the liquid thermal glue, which cools down and solidifies within 15 min. This method helped align the male cartridge part with female PDMS part without developing any mismatch between assembling and disassembling (due to a possible spatial misalignment error). For each sample, tests were carried out three times and the loading forces were recorded with respect to insertion lengths. Various force profiles were analysed as various female adapter parameters were varied. Four different insertion lengths (1 mm, 1.2 mm, 1.4 mm, 1.6 mm), four different diameter values of the female PDMS holes (1.00 mm, 1.15 mm, 1.20 mm, 1.25 mm), and two different PDMS base to curing agent ratios (5:1, 10:1) were used for characterization of plug-n-play assembly and disassembly forces. Please contact the corresponding authors for inquiring about the availability of the chronic plug-n-play wireless devices and the iPhone version of the smartphone app.
Experimental subjects
Adult (25–35 g) male C57BL/6 J and vGAT::IRES-Cre backcrossed to C57BL/6 J mice were group-housed, given access to food pellets and water ad libitum and maintained on a 12 h:12 h light:dark cycle (lights on at 7:00 am). All animals were kept in a sound-attenuated, isolated holding facility in the lab, one week before surgery, post-surgery and throughout the duration of the behavioural assays to minimize stress. All procedures were approved by the Animal Care and Use Committee of Washington University and conformed to US National Institutes of Health guidelines.
Stereotaxic surgery
After the mice were acclimatized to the holding facility for seven to nine days, they were anaesthetized in an induction chamber (4% isolflurane) and placed in a stereotaxic frame (Kopf Instruments, Model 1900) where they were maintained at 1–2% isoflurane. For the inflammation assays, mice were implanted with the microfluidic device into the dorsal striatum (stereotaxic coordinates from bregma (mm): anterior–posterior (AP): + 1.10, medial–lateral (ML): + /−1.50, dorsal–ventral (DV): −4.00). For the DAMGO-mediated locomotor assays, mice were implanted with the microfluidic device above the VTA (stereotaxic coordinates from bregma (mm): AP: −3.10, ML: + /−0.50, DV: −4.25). For the optofluidics experiment, a craniotomy was performed and vGAT-Cre mice were injected with 0.4 µl of AAV5-EF1a-DIO-ChR2(H134)-eYFP (WUSTL Hope Center Viral Core) unilaterally into the BNST (stereotaxic coordinates from bregma (mm): AP: 0.14, ML: + /−0.90, DV: −4.75). Five weeks later, mice were then implanted with the optofluidic device adjacent to the LH (stereotaxic coordinates from bregma: −1.55 AP, + /−1.50 ML, −5.00 mm DV). A standard electrode holder (KOPF 1770) was adapted to implant the microfluidic and optofluidic devices. The implants were secured and affixed with dental cement (C&B Metabond Adhesive Luting Cement, Parkell). All mice were allowed to recover for five days before behavioural testing. Post-surgery, all mice received subcutaneous injections of buprenorphine hydrochloride (0.05 mg kg–1, Reckitt Benckiser Healthcare Ltd.) for pain management, and of ampicillin (50 mg kg–1, Sage Pharmaceuticals) to prevent infection at the implantation site.
Immunohistochemistry
Immunohistochemistry was performed as described in our previous studies8,12,32. In brief, mice were intracardially perfused with 4% paraformaldehyde, and then brains were sectioned (30 μm) and placed in 1X PB until immunostaining. Free-floating sections were washed in 1X PBS for 3 × 10 min intervals. Sections were then placed in blocking buffer (0.5% Triton X-100 and 5% natural goat serum in 1X PBS) for 1 h at room temperature. After blocking buffer, sections were placed in primary antibody (see below) overnight at room temperature. After 3 × 10 min 1X PBS washes, sections were incubated in secondary antibody (see below) for 2 hrs at room temperature, followed by subsequent washes (3 × 10 min in 1X PBS). Subsequently, sections were incubated in NeuroTrace (435/455 blue fluorescent Nissl stain, Life Technologies) for 1 h, followed by 3 × 10 min 1XPBS and 3 × 10 min 1XPB washes. After immunostaining, sections were mounted and coverslipped with Vectashield Hard set mounting medium (Vector Laboratories) and imaged on a Leica TCS SPE confocal microscope (Supplementary Table 4).
Behavioural assays
Open field test (OFT)
OFT was performed as described in Bruchas et. al.12,45 in a sound attenuated room maintained at 23 °C. Lighting was measured and stabilized at 2,000 lux, and performed in the afternoon between 13:00–16:00 hrs. The open field was a 50 × 50 cm2 square enclosure and was cleaned with 70% ethanol between testing trials. For testing, C57Bl6 mice (microfluidic devices were implanted in the VTA as described, n = 7 per group) were placed in the centre of the open field and allowed to roam freely for 60 min. Movements were video recorded and analysed using Ethovision. The centre was defined as a square comprised of 50% the total area of the OFT.
Contraversive rotation/locomotor testing assay
C57Bl6 mice with microfluidic devices implanted above the VTA were placed in the centre of the same arena used for the OFT and allowed to roam freely for 60 min. Wireless infusion of vehicle, DAMGO (500 pmol, 0.5 µl total volume, Tocris), or naloxone hydrochloride (500 ng or 0.5 µl, Tocris) was initiated and movements were video recorded and analysed using Ethovision. Rotations were defined as full 360° revolutions in the path of movement.
Real-time place preference
vGAT-CreBNST-LH:ChR2 animals were placed in a custom-made unbiased, balanced two-compartment conditioning apparatus (52.5 × 25.5 × 25.5 cm) as described previously33,46. On day one, mice were allowed to freely roam the entire apparatus for a 20 min baseline testing. Entry into one compartment triggered photostimulation (10 ms light pulses at 20 Hz every 5 s) while the animal remained in the light-paired chamber. Entry into the other chamber ended the photostimulation. The following day gabazine (10 µM, 0.5 µl total volume, Tocris) was wirelessly administered through replaceable drug cartridges 10 min before the testing. Mice were counterbalanced so that ~50 % received the gabazine on day two, and there was no difference between animals that received the drug on day two or day three. The side paired with photostimulation was counterbalanced across mice and across sessions. Time spent in each chamber and total distance travelled for the entire 20 min trial was measured using Ethovision 10.5 (Noldus Information Technologies). The triggered wireless photostimulation was elicited using a Noldus I/O Box coupled to a GPIO pin on the SimbleeCOM transmitter that wirelessly controlled the photostimulation output of the of the plug-n-play optofluidic device.
Data analysis
Data are expressed as means ± s.e.m. Data were normally distributed, and differences between the groups were determined using independent t-tests or one-way ANOVA followed by post hoc Bonferroni comparisons if the main effect was significant at P < 0.05. Paired t-tests were used in within subject design experiments. Statistical analyses were conducted using Prism 7.0 (GraphPad).
Reporting Summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
The authors declare that all data supporting the results in this study are available within the paper and its Supplementary Information.
Code availability
All BLE firmware is available in the Supplementary Information.
References
Felix-Ortiz, A. C. et al. BLA to vHPC inputs modulate anxiety-related behaviors. Neuron 79, 658–664 (2013).
Jennings, J. H. et al. Distinct extended amygdala circuits for divergent motivational states. Nature 496, 224–228 (2013).
Kramer, R. H., Mourot, A. & Adesnik, H. Optogenetic pharmacology for control of native neuronal signaling proteins. Nat. Neurosci. 16, 816–823 (2013).
McCall, J. G. & Jeong, J.-W. Minimally invasive probes for programmed microfluidic delivery of molecules in vivo. Curr. Opin. Pharmacol. 36, 78–85 (2017).
Sim, J. Y., Haney, M. P., Park, S. I., McCall, J. G. & Jeong, J.-W. Microfluidic neural probes: in vivo tools for advancing neuroscience. Lab. Chip 17, 1406–1435 (2017).
Park, S. et al. One-step optogenetics with multifunctional flexible polymer fibers. Nat. Neurosci. 20, 612–619 (2017).
Canales, A. et al. Multifunctional fibers for simultaneous optical, electrical and chemical interrogation of neural circuits in vivo. Nat. Biotechnol. 33, 277–284 (2015).
Jeong, J.-W. et al. Wireless optofluidic systems for programmable in vivo pharmacology and optogenetics. Cell 162, 662–674 (2015).
McCall, J. G. et al. Preparation and implementation of optofluidic neural probes for in vivo wireless pharmacology and optogenetics. Nat. Protoc. 12, 219–237 (2017).
Hashimoto, M., Hata, A., Miyata, T. & Hirase, H. Programmable wireless light-emitting diode stimulator for chronic stimulation of optogenetic molecules in freely moving mice. Neurophotonics 1, 011002 (2014).
Iwai, Y., Honda, S., Ozeki, H., Hashimoto, M. & Hirase, H. A simple head-mountable LED device for chronic stimulation of optogenetic molecules in freely moving mice. Neurosci. Res. 70, 124–127 (2011).
Kim, T. et al. Injectable, cellular-scale optoelectronics with applications for wireless optogenetics. Science 340, 211–216 (2013).
McCall, J. G. et al. Fabrication and application of flexible, multimodal light-emitting devices for wireless optogenetics. Nat. Protoc. 8, 2413–2428 (2013).
Noh, K. N. et al. Miniaturized, battery-free optofluidic systems with potential for wireless pharmacology and optogenetics. Small 14, 1702479 (2018).
Park, S. I. et al. Soft, stretchable, fully implantable miniaturized optoelectronic systems for wireless optogenetics. Nat. Biotechnol. 33, 1280–1286 (2015).
Shin, G. et al. Flexible near-field wireless optoelectronics as subdermal implants for broad applications in optogenetics. Neuron 93, 509–521 (2017).
Montgomery, K. L. et al. Wirelessly powered, fully internal optogenetics for brain, spinal and peripheral circuits in mice. Nat. Methods 12, 969–974 (2015).
Alam, M., Chen, X. & Fernandez, E. A low-cost multichannel wireless neural stimulation system for freely roaming animals. J. Neural Eng. 10, 066010 (2013).
Ativanichayaphong, T., He, J. W., Hagains, C. E., Peng, Y. B. & Chiao, J.-C. A combined wireless neural stimulating and recording system for study of pain processing. J. Neurosci. Methods 170, 25–34 (2008).
Chang, C.-W. & Chiou, J.-C. A wireless and batteryless microsystem with implantable grid electrode/3-dimensional probe array for ECoG and extracellular neural recording in rats. Sensors 13, 4624–4639 (2013).
Park, S. I. et al. Ultraminiaturized photovoltaic and radio frequency powered optoelectronic systems for wireless optogenetics. J. Neural Eng. 12, 056002 (2015).
Pinnell, R. C., Dempster, J. & Pratt, J. Miniature wireless recording and stimulation system for rodent behavioural testing. J. Neural Eng. 12, 066015 (2015).
Wentz, C. T. et al. A wirelessly powered and controlled device for optical neural control of freely-behaving animals. J. Neural Eng. 8, 046021 (2011).
Yeh, A. J. et al. Wirelessly powering miniature implants for optogenetic stimulation. Appl. Phys. Lett. 103, 163701 (2013).
Massey, L. K. Permeability Properties of Plastics and Elastomers:A Guide to Packaging and Barrier Materials 2nd edn (William Andrew, 2003).
Frank, R., Bronzi, W., Castignani, G. & Engel, T. Bluetooth low energy: an alternative technology for VANET applications. in 2014 11th Annual Conference on Wireless On-demand Network Systems and Services (WONS) 104–107 (IEEE, 2014).
Getting Started with SimbleeCOM v1.0 (RF Digital Corp, 2015).
Jenck, F., Bozarth, M. & Wise, R. A. Contraversive circling induced by ventral tegmental microinjections of moderate doses of morphine and [D-Pen2, D-Pen5]enkephalin. Brain Res. 450, 382–386 (1988).
Devine, D. P. & Wise, R. A. Self-administration of morphine, DAMGO, and DPDPE into the ventral tegmental area of rats. J. Neurosci. 14, 1978–1984 (1994).
Namburi, P., Al-Hasani, R., Calhoon, G. G., Bruchas, M. R. & Tye, K. M. Architectural representation of valence in the limbic system. Neuropsychopharmacology 41, 1697–1715 (2016).
Jennings, J. H., Rizzi, G., Stamatakis, A. M., Ung, R. L. & Stuber, G. D. The inhibitory circuit architecture of the lateral hypothalamus orchestrates feeding. Science 341, 1517–1521 (2013).
Al-Hasani, R. et al. Distinct subpopulations of nucleus accumbens dynorphin neurons drive aversion and reward. Neuron 87, 1063–1077 (2015).
McCall, J. G. et al. CRH Engagement of the locus coeruleus noradrenergic system mediates stress-induced anxiety. Neuron 87, 605–620 (2015).
Dagdeviren, C. et al. Miniaturized neural system for chronic, local intracerebral drug delivery. Sci. Transl. Med. 10, eaan2742 (2018).
Spieth, S., Schumacher, A., Kallenbach, C., Messner, S. & Zengerle, R. The neuromedicator—a micropump integrated with silicon microprobes for drug delivery in neural research. J. Micromech. Microeng. 22, 065020 (2012).
Minev, I. R. et al. Electronic dura mater for long-term multimodal neural interfaces. Science 347, 159–163 (2015).
Qiu, Y. & Park, K. Environment-sensitive hydrogels for drug delivery. Adv. Drug Deliv. Rev. 53, 321–339 (2001).
Jang, K.-I. et al. Soft network composite materials with deterministic and bio-inspired designs. Nat. Commun. 6, 6566 (2015).
Liu, Y. et al. Epidermal mechano-acoustic sensing electronics for cardiovascular diagnostics and human-machine interfaces. Sci. Adv. 2, e1601185 (2016).
Banghart, M. R. & Sabatini, B. L. Photoactivatable neuropeptides for spatiotemporally precise delivery of opioids in neural tissue. Neuron 73, 249–259 (2012).
Tochitsky, I. et al. Restoring visual function to blind mice with a photoswitch that exploits electrophysiological remodeling of retinal ganglion cells. Neuron 81, 800–813 (2014).
Banala, S. et al. Photoactivatable drugs for nicotinic optopharmacology. Nat. Methods 15, 347–350 (2018).
Mehrabian, A. & Abousleiman, Y. General solutions to poroviscoelastic model of hydrocephalic human brain tissue. J. Theor. Biol. 291, 105–118 (2011).
Liu, Q., Wang, Z., Lou, Y. & Suo, Z. Elastic leak of a seal. Extrem. Mech. Lett. 1, 54–61 (2014).
Bruchas, M. R., Land, B. B., Lemos, J. C. & Chavkin, C. CRF1-R activation of the dynorphin/kappa opioid system in the mouse basolateral amygdala mediates anxiety-like behavior. PLoS ONE 4, e8528 (2009).
Siuda, E. R. et al. Spatiotemporal control of opioid signaling and behavior. Neuron 86, 923–935 (2015).
Acknowledgements
This work was supported by the Basic Science Research Program through the National Research Foundation of Korea funded by the Ministry of Science and ICT (grant nos. NRF-2018R1C1B6001706 and NRF-2018025230, J.-W.J.). This work was also supported by Mallinckrodt Professorship (M.R.B.), NIH (grant no. R01DA037152), NIDA Diversity Supplement (grant no. R01DA033396-S1, M.R.B. and A.G.), and grant no. NIDA F32DA043999 (D.C.C). Support was also provided by the Hope Center Viral Vectors Core. We thank J.-W. Yu (KAIST) for providing equipment to conduct BLE wireless transmission tests.
Author information
Authors and Affiliations
Contributions
R.Q., A.G., M.R.B. and J.-W.J. conceptualized the project and designed the experiments with methodology. R.Q., J.A. and A.A. fabricated and prepared the devices for behavioural tests. R.Q., A.G. and D.C.C. performed the in vivo behavioural, tracing and imaging experiments. R.Q., A.G., Z.Z., J.X., J.Y.S., C.Y.K., S.-H.B., B.C.L., K.I.J., J.X., M.R.B. and J.-W.J. performed the investigation, analysed the data and wrote up the modelling results. R.Q., Y.X., A.A. and F.L., designed the firmware and software. R.Q., A.G., D.C.C, M.R.B. and J.-W.J. wrote the paper. M.R.B. and J.-W.J. acquired funding and supervised the project. M.R.B. and J.-W.J. are co-senior authors.
Corresponding authors
Ethics declarations
Competing interests
M.R.B. is a co-founder and scientific advisor for Neurolux, Inc., a neurotechnology company that offers neuroscience tools. The device described in this study is not currently sold or manufactured by this company.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary methods, figures, tables and video captions.
Supplementary Video 1
Highly precise and wirelessly reprogrammable temporal control for the sequenced delivery of two distinct fluids, with a 1 s delay in between.
Supplementary Video 2
Wireless operation of the plug-n-play optofluidic device.
Supplementary Video 3
Spatiotemporal heat analysis during fluid actuation using the IR camera.
Supplementary Video 4
Smartphone App Graphical User Interface for the wireless, selective and programmable control of multimodal plug-n-play optofluidic devices.
Supplementary Video 5
Demonstration of a dependent closed-loop concept through the SimbleeCOM Protocol, using model mice.
Supplementary Video 6
Wireless chronic drug delivery in a freely moving mouse.
Supplementary Video 7
Wireless selective control triggering of intra-VTA DAMGO release in a group of four mice during a 60-min open-field test.
Rights and permissions
About this article
Cite this article
Qazi, R., Gomez, A.M., Castro, D.C. et al. Wireless optofluidic brain probes for chronic neuropharmacology and photostimulation. Nat Biomed Eng 3, 655–669 (2019). https://doi.org/10.1038/s41551-019-0432-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41551-019-0432-1
This article is cited by
-
Multilayer stretchable electronics with designs enabling a compact lateral form
npj Flexible Electronics (2024)
-
Design and validation of a low-cost photomodulator for in vivo photoactivation of a mGluR5 inhibitor
Biomedical Engineering Letters (2024)
-
Wearable and Implantable Light-Emitting Diodes and Their Biomedical Applications
Korean Journal of Chemical Engineering (2024)
-
Recent developments in multifunctional neural probes for simultaneous neural recording and modulation
Microsystems & Nanoengineering (2023)
-
Customizable, wireless and implantable neural probe design and fabrication via 3D printing
Nature Protocols (2023)