Abstract
Antimicrobial compounds are essential for controlling bacterial infections. Stress-induced bacterial tolerance and persisters can undermine antimicrobial activities under laboratory conditions, but their quantitative effects under physiological conditions remain unclear1,2. Here we determined constraints on clearance of Salmonella by antimicrobials in infected mice and tissue-mimicking chemostats. The antibiotics enrofloxacin and ceftriaxone exhibited poor anti-Salmonella activity under both conditions, primarily owing to severe nutrient starvation, which restricted Salmonella replication3,4,5. Other infection-associated conditions, such as acidic pH, glucose, oxidative stress, nitrosative stress, antimicrobial peptides, osmolarity, oxygen limitation, carbon dioxide and carbonate, as well as drug efflux, toxin–antitoxin modules and cell size had limited effects. A subset of resilient Salmonella appeared as a key obstacle for clearance by enrofloxacin, based on the biphasic decline of Salmonella colony-forming units. However, these data were misleading, because colony formation was confounded by extensive post-exposure killing. More accurate single-cell, real-time assays showed uniformly slow damage, indicating high resilience across the entire Salmonella population. The resulting extensive survival of bulk bacteria minimized the effect of hyper-resilient persisters. Thus, starvation-induced general resilience of Salmonella was the main cause of poor antibiotic clearance. These findings highlight the importance of quantifying antibiotic activity with real-time, single-cell assays under physiological conditions.
Similar content being viewed by others
Main
Effective antimicrobial therapy is crucial for control of bacterial infections. Antimicrobial resistance can impede treatment success, but eradication failures occur even in the absence of resistance6. These failures are often attributed to host stresses that trigger bacterial drug tolerance1 and/or subsets of bacteria, such as persisters, that are refractory to killing2. Supporting evidence comes mostly from laboratory conditions, and the relevance under physiological conditions remains unclear. Here we determined the quantitative effect of bacterial stresses and heterogeneity on antimicrobial efficacy in a mouse model of invasive salmonellosis, a difficult-to-treat infection that affects around 15 million patients and causes around 200,000 deaths annually7. Our mouse model replicates treatment failures observed in humans8 and exposes Salmonella to diverse stresses, leading to the formation of heterogeneous bacterial subsets with divergent properties and fates9,10. Thus, the model is suitable for assessing the effects of host stresses and bacterial heterogeneity on antimicrobial clearance in a clinically relevant context.
Inefficient killing of Salmonella
We infected genetically susceptible mice with gfp-expressing Salmonella enterica subsp. enterica serovar Typhimurium. Upon appearance of clinical symptoms, we administered the recommended dose of 5 mg per kg (body weight) enrofloxacin (the widely used veterinary version and prodrug of ciprofloxacin), which is distributed organism-wide11 within approximately 10 min. After 1 h, we euthanized the mice and recovered an approximately 20-fold diminished number of Salmonella colony-forming units (CFUs) from the major target organ spleen12. This CFU loss was around 300-fold slower compared with standard laboratory conditions for antimicrobial susceptibility testing (exponential growth in Mueller–Hinton broth under normoxia at 37 °C) with an equivalent enrofloxacin concentration12 (1.5 mg l−1) (Fig. 1a). Similarly, a dose of 50 mg kg−1 ceftriaxone diminished CFUs in spleen approximately 8-fold over 4 h, around 40-fold slower than under standard laboratory conditions with 25 mg l−1 ceftriaxone. Thus, the two recommended bactericidal antibiotic classes for treatment of invasive salmonellosis (fluoroquinolones and cephalosporins)7 had poor anti-Salmonella activity in infected mice, consistent with slow antimicrobial clearance in humans13. This was not owing to the emergence of resistance, because Salmonella from treated mice12 and humans retain full susceptibility. Slow clearance is the primary reason for eventual treatment failures because some Salmonella still survive in host tissues when the critical support of host inflammation vanishes12.
a, Salmonella survival in mouse spleen after an antibiotic dose (grey symbols show re-analysed data from ref. 12; enrofloxacin (ENR): 1 h, n = 10; 2 h, n = 3; 4 h, n = 6; ceftriaxone (CRO), n = 6) or in Mueller–Hinton broth under normal atmosphere at 37 °C (red symbols (this study); enrofloxacin, n = 5; ceftriaxone, n = 3). Each symbol represents an individual mouse or an independent in vitro culture. Lines connect the geometric means. Two-tailed t-test of log-transformed data. b, Salmonella survival in tissue-mimicking chemostat cultures (grey symbols show re-analysed data from ref. 12; enrofloxacin: 1 h and 2 h, n = 12; 4 h, n = 7; ceftriaxone 1 h, 2 h and 4 h, n = 4) or laboratory conditions (red symbols; number of samples as in a). Each symbol represents an individual chemostat reactor. Lines connect the geometric means. Two-tailed t-test of log-transformed data. c, Survival of wild-type (WT) and indicated mutant Salmonella in spleen. Each symbol represents an individual mouse (enrofloxacin: wild type and lexA3 1 h, n = 3; wild type 4 h, n = 3; tisB, n = 4; Δ3T, n = 3; ceftriaxone: wild type and Δ3T, n = 6). Horizontal bars represent geometric means. Enrofloxacin, one-way ANOVA of log-transformed data with comparisons to wild-type data and Holm–Šídák correction for multiple comparisons; ceftriaxone, two-tailed t-test of log-transformed data. d, Survival of wild-type and indicated mutant Salmonella in chemostat cultures. Each symbol represents an individual chemostat reactor (enrofloxacin: wild type and lexA3 1 h, n = 5; wild type 4 h, n = 16; tisB and Δ3T, n = 4; ceftriaxone: wild type, n = 8; Δ3T, n = 7). Horizontal bars represent geometric means (statistical tests as in c).
Limited effect of diverse stresses
To identify constraints on anti-Salmonella activities, we mimicked the extensively characterized Salmonella tissue microenvironments in chemostats. We used 10% oxygen, 5% carbon dioxide balanced with 10 mM bicarbonate at pH 5.6, and 23 nutrients available to Salmonella in the mouse spleen5. We set the inflow of fresh medium to 0.116 ml h−1 per ml of culture, mimicking the severe nutrient starvation that limits Salmonella growth in mice3 (approximately 0.16 divisions per hour, generation time approximately 6 h). Under these conditions, physiological concentrations of enrofloxacin12 (1.5 mg l−1) or ceftriaxone14 (25 mg l−1) killed Salmonella at rates similar to those in mice (Fig. 1b). A lexA3 allele, which blocks repair of DNA double-strand breaks (DSBs)15, accelerated enrofloxacin killing approximately 100-fold in mice and chemostats (Fig. 1c,d), indicating that enrofloxacin triggered DSBs (which are lethal without repair) in almost all Salmonella, consistent with pharmacological target attainment12 under both conditions. Toxins encoded by tisB16 or ecnB3, shpAB and phD-doc17 (deleted in Δ3T), had no detectable effects on enrofloxacin and ceftriaxone activities in mice and chemostats18 (Fig. 1c,d). In summary, tissue-mimicking chemostats recapitulated the poor in vivo activities of both antibiotics.
To identify factors that constrained antibiotic activity in the chemostat experiments, we varied tissue-associated stresses that are known to affect fluoroquinolone efficacy, including acidic pH, reduced oxygen tension, increased carbon dioxide tension and bicarbonate concentration, osmolarity, glucose, oxidative stress and membrane-damaging antimicrobial peptides (Supplementary Note 1). We also inactivated AcrB, the main efflux pump for fluoroquinolones19 and a proposed cause of delayed antimicrobial clearance20, and compared Salmonella cells with different cell size or cell age21 (Extended Data Fig. 1a). Some of these parameters affected Salmonella killing by enrofloxacin, but the effects were generally small (up to threefold; glucose has an approximately sixfold effect) compared with the approximately 300-fold difference from standard laboratory conditions (Fig. 2a), consistent with their moderate effects under other in vitro conditions (Supplementary Note 1). Oxidative and nitrosative stresses were not required for poor enrofloxacin and ceftriaxone activities, consistent with their minor effects in vitro (Supplementary Note 1) and in mice (Supplementary Note 2). Combining conditions that promote survival (pH 5.6; 5% CO2/10 mM bicarbonate; 0.4% glucose; 401 mOsm) resulted in approximately fivefold greater survival (Fig. 2a, yellow circles). Unknown stresses or stress combinations may exist in vivo, but our results indicate the presence of a non-stress factor that dominates the high in vivo-like Salmonella survival in chemostats.
a, Salmonella survival after 1 h exposure to enrofloxacin in chemostat cultures with varying conditions. Each symbol represents an individual chemostat reactor. P values adjusted for multiple comparisons (Holm–Šídák) (two-tailed t-test on log-transformed data for pH; ANOVA on log-transformed data for glucose and osmolarity). BIC, bicarbonate; CS, combined stresses; MHB, Mueller–Hinton broth; Std, standard tissue-mimicking conditions. b, Survival of Salmonella in mice (squares, geometric mean ± geometric s.d.; enrofloxacin: Slc11a1s/WT, n = 10; Slc11a1s/hipAD88N, n = 4; Slc11a1r/WT, n = 8; ceftriaxone, n = 6), or in chemostats in tissue-mimicking medium (geometric mean ± geometric s.d.; enrofloxacin for division rates 0.083 h−1, 0.17 h−1 and 0.33 h−1, n = 10; ceftriaxone, n = 4), Mueller–Hinton broth (enrofloxacin or ceftriaxone for division rates 0.083 h−1, 0.17 h−1 and 0.33 h−1, n = 5) or in individual batch cultures (enrofloxacin: tissue-mimicking medium, n = 3; Mueller–Hinton broth, n = 5; ceftriaxone: tissue-mimicking medium and Mueller–Hinton broth, n = 3). One-way ANOVA with test for linear trend for log-transformed data for tissue-mimicking medium or Mueller–Hinton broth cultures. c, Relationship between exposure time to ceftriaxone to number of generations and Salmonella survival for different proliferation rates and exposure times (geometric mean and geometric s.d.; upward triangles, division rate 0.17 h−1 and exposure for 1 h (n = 4), 2 h (n = 4) or 4 h (n = 9); downward triangles, 4 h exposure and division rates 0.08 (n = 5) or 0.33 h−1 (n = 5)). The dashed line represents a monoexponential fit and the shaded area shows the 95% confidence interval.
To determine the role of nutrient access, we grew Salmonella in low-density batch cultures, keeping all other parameters the same as in tissue-mimicking chemostats. Facile nutrient access under these conditions led to approximately tenfold faster replication (around 1.5 divisions per hour) and increased killing by enrofloxacin and ceftriaxone by about 200-fold (Fig. 2a,b), highlighting the critical role of nutrient access in antibiotic killing. Multiple linear regression of the data shown in Fig. 2a, with survival as dependent variable and nutrient access (which controlled the replication rate), oxygen, pH, CO2, glucose, LL-37, osmolarity and H2O2 as independent variables, explained 90.4% (R2) of the variance in survival (Extended Data Table 1). Nutrient access and replication rate (P < 10−15), osmolarity (P = 8.6 × 10−7) and H2O2 (P = 0.020) had a significant effect; of these factors, nutrient access and replication rate had by far the largest effect size (165-fold versus 3-fold (osmolarity) and 1.5-fold (H2O2); Fig. 2a). Thus, nutrient access controlling replication rate dominated antibiotic survival.
To confirm this, we starved Salmonella under non-physiological stress-free conditions (Mueller–Hinton broth, pH 7.4, normoxia) in chemostats, limiting Salmonella nutrition by slow medium inflow to achieve ~0.16 divisions per hour, as seen in vivo3. These conditions resulted in high Salmonella survival (approximately 3% after 1 h of enrofloxacin and 30% after 4 h of ceftriaxone; Fig. 2a–c) as in mice, indicating that starvation at levels similar to those experienced by Salmonella in mice3,5 was sufficient to achieve in vivo-like antibiotic survival rates, even under non-physiological, stress-free conditions. This was consistent with previous evidence linking starvation and slow replication with increased resilience against antibiotic activity18,22.
To determine the effect of replication rate in mice, we used two different approaches. First, we expressed the Escherichia coli toxin gene hipA in Salmonella. HipA inhibits translation and replication by phosphorylating GltX, but this can be prevented by the antitoxin HipB23. When HipA and HipB levels are similar, fluctuations create a bimodal distribution of growing ([HipA] < [HipB]) and non-growing ([HipA] > [HipB]) cells23. Without HipB, HipA impairs growth but does not create this heterogeneity. We expressed the partially detoxified allele24 hipAD88N in Salmonella (which naturally lacks hipAB). This did not affect the enrofloxacin mean inhibitory concentration (MIC) (0.06 mg l−1), but reduced the replication rate in vitro (to around 47%) and in vivo (to around 71%; Extended Data Fig. 1b,c; competitive index in mice at day 4 post-infection, 0.028 ± 0.009, n = 6, P = 4 × 10−5, one-sample t-test of log-transformed data). In mice, Salmonella hipAD88N survived enrofloxacin exposure around threefold better than parental Salmonella (Fig. 2b and Extended Data Fig. 1d). In a second approach, we tracked Salmonella killing in Slc11a1r mice, which encode an active metal transporter SLC11A1 (also known as NRAMP1)4. SLC11A1 deprives Salmonella of magnesium, reducing its replication rate to around 50% of that in standard laboratory mice (Slc11a1s) with dysfunctional SLC11A1 (Extended Data Fig. 1c) without affecting stress levels or access to most other nutrients4. In Slc11a1r mice infected with wild-type Salmonella, we observed around 15% CFU recovery after 1 h enrofloxacin treatment (approximately fourfold more than in Slc11a1s mice; Fig. 2b and Extended Data Fig. 1d). Plating on low-nutrient minimal medium—which improves CFU recovery (see below)—resulted in a 1 h survival rate of about 32% (n = 4) in Slc11a1r mice. This high survival is physiologically relevant because humans and wild mice carry Slc11a1r. Thus, slowing Salmonella replication in vivo using two different methods significantly increased antibiotic survival consistent with the growth–killing relationship observed in vitro.
These data indicate that the scarcity of carbon and energy sources (standard laboratory Slc11a1s mice) and magnesium (in Slc11a1r mice), which limit Salmonella replication4,5, are the primary cause of Salmonella resilience to antibiotics in vivo. This resilience could be owing to reduced DNA replication and cell wall synthesis (the targets of fluoroquinolones and cephalosporins) at slow growth and/or metabolic effects of limited nutritients25. Further research is required to disentangle these mechanisms.
Biphasic loss of CFUs
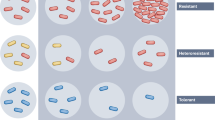
Ceftriaxone killed Salmonella continuously by 0.90 ± 0.14 log per generation (Fig. 2c), suggesting slow loss of viability across the entire Salmonella population26. By contrast, enrofloxacin killed around 95% of Salmonella within the first 1 h of exposure (killing rate approximately 3 h−1) (Fig. 1a,b), and the remaining 5.4 ± 1.8% (in vivo) or 7.4 ± 3.3% (chemostat) lost viability at a slower rate over the next 3 h (killing rate 0.35 h−1). These biphasic kinetics suggested that a subset of 5–7% resilient Salmonella was a key obstacle for enrofloxacin-induced clearance in mice and in chemostats (antibiotic persistence)2.
According to consensus guidelines2, antibiotic persistence is measured by exposing bacteria to antibiotics for various time intervals, followed by washing and plating on agar plates. After overnight incubation, colonies are counted and the data are plotted against exposure time. A biphasic decline of CFUs (as observed here; Fig. 1a,b) is considered to be evidence that not all bacteria in the population are killed at the same rate. However, this strategy uses a late and indirect readout (colony formation overnight) to infer killing kinetics during antibiotic exposure, and relies on the assumption that each bacterium that is viable at the time of plating will form a colony. This assumption is violated in diverse pathogen–antibiotic combinations (Supplementary Note 3), indicating a need for more direct, real-time readouts of antimicrobial activity.
Slow monophasic DNA damage
To monitor enrofloxacin activity in real-time, we detected DSBs, the crucial initial damage of fluoroquinolone action27, using Salmonella expressing a recAR29A-mCherry fusion. RecA–mCherry forms visible foci around all newly formed DSBs within <4 min (refs. 28,29) without interfering with subsequent DNA repair29,30. The R29A mutation prevents DSB-independent RecA aggregation31. Formation of RecA foci relies on the diffusion of constitutively present proteins with no need for de novo gene expression. RecA foci, therefore, serve as an early, sensitive, and reliable readout for DSBs before the initiation of SOS response and DNA repair28,29,30,31. Expressing recAR29A-mCherry from the PrecA promoter provides basal RecA–mCherry for visualizing emerging DSBs, and increasing RecA–mCherry levels during the subsequent SOS response (Extended Data Fig. 1e).
We imaged Salmonella expressing recAR29A-mCherry in a microfluidic device during slow growth in tissue-mimicking, nutrient-poor medium. RecA–mCherry occasionally formed short-lived (less than 5 min) foci (Fig. 3a) indicating spontaneous, rapidly repairable damage during chromosomal replication29. Long-lasting RecA foci (lasting more than 5 min; Fig. 3a), indicating more persistent DSBs28, occurred at a rate of around 0.03 h−1 (Extended Data Fig. 1f), mostly without triggering a subsequent SOS response. These data were consistent with slow baseline DNA damage in untreated bacteria29,31.
a, Time-lapse gallery of RecA foci in enrofloxacin-exposed Salmonella. Scale bar, 1 μm. b, Snapshots of Salmonella exposed for 1 h to enrofloxacin, followed by drug washout for 30 min and incubation in LB. Scale bar, 5 μm. c, Fraction of undamaged and regrowing cells during 1 h (top), 2 h (middle) or 4 h (bottom) enrofloxacin exposure, washout and LB incubation (250 (top), 255 (middle) and 250 (bottom) cells; dotted lines show monoexponential fits for damage during exposure and washout; summary data and independent replicates in d,g). d, Fractions of undamaged cells at the end of enrofloxacin exposure, in LB, and regrowing survivors (two independent experiments, 755 and 1,233 cells). e, Snapshots of Salmonella exposed for 7 h to decreasing concentrations of enrofloxacin, followed by drug-free nutrient-poor medium (Supplementary Video 3). Scale bar, 5 μm. f, Fraction of undamaged and regrowing cells during and after 7 h exposure to decreasing concentrations of enrofloxacin (ENR) in nutrient-poor medium (276 cells; dotted lines show monoexponential fits for damage during exposure, post-antibiotic damage or baseline damage; summary data for this and two independent replicates in g). g, Fractions of regrowing cells after 4 h enrofloxacin exposure and a switch to LB (4 h/LB; 250 and 444 cells; same data as in d) or under in vivo-mimicking conditions (IVM) with declining enrofloxacin concentrations and regrowth in nutrient-poor medium (276, 271 and 378 cells). Circles represent independent experiments. Two-tailed t-test on log-transformed data. h, Fluorescence of Salmonella/pPcad-gfp or Salmonella lexA3/pPcad-gfp in untreated (0 h) or enrofloxacin-treated mice. The vertical line separates GFP+ responders from GFP− non-responders. The inset shows the median fluorescence (MFI) of GFP+ cells, the line connects the geometric means (test for non-zero slope in a linear regression of log-transformed values). The histograms represent pooled data, circles in the inset graph represent individual mice (1 h, n = 5; 3 h and 4 h, n = 4). i, Blue, fraction of GFP− non-responders in enrofloxacin-treated mice (0 h, n = 2; 1 h, n = 6; 2 h and 4 h, n = 4). Each symbol represents an individual mouse. Brown, CFUs recovered from similar samples (same data as in Fig. 1a; geometric mean ± geometric s.d.; 1 h, n = 10; 2 h, n = 3; 4 h, n = 6). Two-way ANOVA for difference between SOS response and CFU recovery. j, Contribution of responders (SOS+) and non-responders (SOS−) to CFU counts (Supplementary Note 5; data are mean ± s.d. for data from independently infected mice; 1 h, n = 6; 4 h, n = 4). Two-way ANOVA for difference between SOS+ and SOS−.
Exposure to 1.5 mg l−1 enrofloxacin accelerated formation of long-lasting RecA foci to around 0.21 h−1 (Extended Data Fig. 1f). Each focus was followed by a SOS response, indicating severe DNA damage. The fraction of ‘undamaged’ cells (those that had not yet experienced any DSB), declined monoexponentially to around 40% after 4 h of enrofloxacin exposure. These real-time data were inconsistent with the CFU data because: (1) only around 15% cells experienced the critical primary DSB within 1 h of exposure, yet plating such cells showed a 20-fold decrease in CFU (Fig. 1a,b); and (2) damage was monoexponential, whereas the decrease in CFU was biexponential. The discrepancies were not explained by insufficient enrofloxacin exposure in the microfluidic device (for example, due to drug absorption in the microfluidic device), because increasing enrofloxacin concentration to 5 mg l−1 had only a minor effect on damage kinetics (Extended Data Fig. 1f), consistent with nearly saturating enrofloxacin exposure12 (we used 5 mg l−1 for all subsequent experiments). The discrepancies were not caused by filamentation of enrofloxacin-exposed bacteria, which might make them more prone to pipetting damage, because Salmonella in low-nutrient medium and in mice did not form filamented cells during enrofloxacin exposure (Extended Data Fig. 1g and Supplementary Video 2). The discrepancies were also not caused by insufficient sensitivity of DSB detection, because each SOS-responding cell had previously exhibited a long-lasting RecA focus, indicating comprehensive detection of relevant DNA damage28,29,31. RecA forms foci around all newly formed DSBs within minutes28, arguing against relevant delays in detection of the DNA damage. Thus, DNA damage during exposure was inconsistent with CFU data.
Massive post-exposure damage
The discrepancies might arise during post-exposure regrowth on lysogeny broth (LB) agar plates until visible colonies form. We first assessed the effect of switching from nutrient-poor medium to LB without prior antibiotic exposure (simulating regrowth of untreated Salmonella on LB plates). Switching to LB triggered a burst of long-lasting RecA foci in around 40% of cells, suggesting substantial DNA stress in the initial 10 min after nutrient upshift (‘nutrient shock’32) (Extended Data Fig. 1h,i and Supplementary Video 1). However, only few of these events triggered SOS responses and around 98% of DSB+ cells restarted division after a lag of 1.5 h on LB in synchrony with undamaged DSB− cells (Extended Data Fig. 1h–j and Supplementary Video 1), indicating efficient repair and negligible fitness loss.
We then simulated the entire CFU assay by exposing Salmonella for 1, 2 or 4 h to enrofloxacin in nutrient-poor medium, followed by drug washout for 30 min with antibiotic-free nutrient-poor medium, and regrowth in LB. Under these conditions, the shift to LB triggered vigorous RecA localization dynamics and SOS responses for several hours in all analysed cells, indicating severe DNA damage after the actual antibiotic exposure (Fig. 3b,c and Supplementary Video 2). Almost all cells increased in size, and many formed long filaments. Some cells reinitiated cell division about 3.5 h after the initial DSB (Extended Data Fig. 1j) and formed expanding microcolonies, indicating successful DNA repair. The frequency of these survivors (Fig. 3c,d, 1 h enrofloxacin exposure, about 10% survival; 4 h, about 3% survival) was similar to CFU data from enrofloxacin-treated chemostat cultures (Fig. 1b, 1 h, about 7% survival; 4 h, about 2% survival). Thus, enrofloxacin induced DSBs and killed Salmonella primarily post-exposure during regrowth on LB, explaining the discrepancy between limited damage during exposure and low CFU recovery.
Nutrient-rich LB is a poor mimic of relevant regrowth conditions in tissues. To approximate the in vivo situation, we grew Salmonella in nutrient-poor medium, exposed them to diminishing enrofloxacin concentrations approximating enrofloxacin pharmacokinetics in mice11, and maintained them in nutrient-poor medium after exposure. Under these conditions, Salmonella exhibited long-lasting RecA foci with monoexponential kinetics at 0.18 h−1 throughout the 7 h of enrofloxacin exposure and about 1 h after washout, followed by slower monoexponential kinetics at 0.07 h−1 for around 14 h in drug-free medium. Thereafter, focus formation returned to the basal rate of 0.02 h−1 (Fig. 3e,f and Supplementary Video 3). All cells with long RecA foci showed vigorous SOS responses and RecA localization dynamics indicating severe DNA damage. However, growth and filamentation were less extensive than in LB. Re-initiation of division and formation of microcolonies started 4 to 30 h after the initial DSB (Extended Data Fig. 1j), and around fivefold more cells survived than in 4 h exposure followed by LB regrowth (Fig. 3g), despite more damage at the end of exposure. Thus, scarce nutrition improved repair and survival, reaching levels (14 ± 4%; regrowing survivors) consistent with Salmonella loads in the spleen 24 h after enrofloxacin doses (34 ± 13% of pre-dose levels; this includes regrowing survivors and their daughter cells)12.
Together, our results demonstrate that enrofloxacin continued to damage Salmonella after the end of exposure. This was consistent with the half-life of ternary enrofloxacin–gyrase–DNA complexes of 2.5 h causing extended post-exposure growth inhibition (post-antibiotic effect)33. A shift to nutrient-rich LB caused extensive DSBs, explaining the need for DNA repair after, but not during, fluoroquinolone exposure in CFU assays15,34. Vigorous growth of enrofloxacin-poisoned cells on LB might cause biosynthetic imbalances that lead to viability loss35. Physiological starvation slowed regrowth3,5, resulting in less damage and allowing more time for repair.
These findings indicated that plotting CFU against exposure time was misleading, because most viability loss occurred not during exposure (as implicitly assumed in CFU-based assays), but after exposure. Thus, the approximately 20-fold drop in CFU on LB plates after 1 h of exposure did not represent the killing of 95% of the Salmonella population within that 1 h, and the gradual CFU decline with extended exposure did not indicate a refractory subpopulation. Instead, enrofloxacin exposure itself inflicted slow damage, but around 90% of the yet undamaged, enrofloxacin-poisoned Salmonella died post-exposure during regrowth, irrespective of prior exposure times (Fig. 3d and Extended Data Fig. 2a). Thus, the biphasic CFU kinetics did not reflect heterogeneous antibiotic survival but rather a confounded viability readout.
Real-time imaging revealed slow, monoexponential damage of Salmonella by enrofloxacin, suggesting low but uniform and constant damage probabilities for individual cells (akin to the radioactive decay of unstable atomic nuclei). Thus, the entire Salmonella population, and not just a small subset, was rather refractory to enrofloxacin-inflicted damage. Some damaged Salmonella were able to repair the DSBs and survived, further delaying clearance. We cannot exclude that some cells had lower damage probabilities or superior repair capabilities, but even the bulk population died at rates below 0.2 h−1.
Slow monophasic SOS responses in mice
We next investigated Salmonella killing in mice. Detecting in vivo DNA damage by tracking RecA foci over hours is challenging in mouse tissues. Instead, we monitored the Salmonella SOS response to DNA damage using a reporter strain carrying a sensititve Pcad-gfp fusion36 (Extended Data Fig. 2b,c). In the spleen of mice, the reporter showed negligible SOS activity before enrofloxacin administration (Fig. 3h), indicating limited host-induced DSBs (in contrast to infections of macrophages in cell culture; Supplementary Note 4).
Enrofloxacin administration activated around 25% Salmonella SOS reporter cells within 1 h (Fig. 3h,i). This was a specific SOS response, because SOS-defective Salmonella lexA3 carrying the same reporter construct showed no response. Prolonged in vivo exposure to enrofloxacin increased the brightness and proportion of SOS+ Salmonella cells, resulting in a monoexponential decay of non-responders (SOS−) at a rate of 0.24 h−1. Non-responders retained a functional reporter construct and experienced enrofloxacin poisoning in vivo, because most reporter cells exhibited a SOS response post-exposure upon ex vivo incubation in LB15 (Extended Data Fig. 2d). Ex vivo sorting and plating of SOS+ and SOS− Salmonella revealed that most colonies originated from SOS− Salmonella cells that had not yet responded in vivo (Fig. 3j, Extended Data Fig. 2e and Supplementary Note 5). These observations were inconsistent with the CFU data because: (1) after 1 h of exposure only around 25% Salmonella responded to DNA damage, whereas the CFU dropped around 20-fold; (2) the response to DNA damage was monoexponential, whereas the CFU decline was biexponential; (3) most colonies originated from in vivo non-responders (SOS−), although an active SOS response was essential for formation of more than 99% of all colonies (based on the phenotype of SOS-deficient Salmonella lexA3; Fig. 1c). These data suggested that most DNA damage, SOS response and viability loss occurred after enrofloxacin exposure during regrowth on LB (Extended Data Fig. 2a), consistent with our observations in microfluidic devices (Fig. 3d).
To test the idea that regrowth on LB compromised the colony-forming ability of initially viable but enrofloxacin-poisoned Salmonella, we explored alternative plating media to reduce post-exposure damage. The addition of thiourea and dipyridiyl to mitigate oxidative stress had no effect on colony recovery, consistent with oxygen-independent killing by second-generation fluoroquinolones at concentrations achieved in vivo12,37. Lowering the incubation temperature diminished colony counts. Plating on the nutrient-poor medium used in the microfluidics devices yielded no visible colonies even after 7 days of incubation. However, after increasing carbon and energy sources tenfold, this medium supported formation of tiny colonies after 3 days at 37 °C. Plating spleen homogenates from enrofloxacin-treated mice on this medium yielded 2.2 ± 0.4-fold higher CFU than on LB (11 independent infections, P < 0.0001, two-tailed t-test on log-transformed values). This confirmed that a majority of enrofloxacin-poisoned but initially alive Salmonella died on LB plates, whereas some of them could repair the DNA damage and survive during slow regrowth on nutrient-poor medium34. The nutrient-poor medium and standard LB yielded similar CFU for Salmonella from untreated control mice (3 infections; 1.1 ± 0.1; P = 0.19), indicating that slow growth enhanced specifically the survival of enrofloxacin-poisoned Salmonella (as in microfluidic devices; Fig. 3g). Further optimization of regrowth conditions might yield even higher CFUs from enrofloxacin-treated mice, but they would still underestimate the number of initially alive Salmonella owing to inevitable post-exposure damage by still-bound enrofloxacin (Fig. 3f). Thus, CFU data would remain a confounded readout.
The slow monoexponential SOS kinetics (Fig. 3i) suggested that enrofloxacin damaged Salmonella in vivo with low but rather homogenous and constant single-cell probabilities. Thus, the Salmonella bulk population, rather than only a minor persister subset, was highly refractory to DNA damage. Against this background of high resilience and massive survival, minor subsets with even superior survival would have limited impact. This was consistent with the only about threefold clearance per day during a 4-day treatment with daily enrofloxacin administration12. A Salmonella subset with even slower clearance exists in the splenic white pulp. This subset experiences sufficient enrofloxacin exposure, but insufficient local inflammation provides inefficient support for antibiotic clearance. Eventually, inflammation resolves across the entire spleen, resulting in overall eradication failure. By contrast, sustaining inflammation throughout antimicrobial treatment enables eradication from all spleen compartments, confirming the central role of the host immune system and the limited effect of nonreplicating Salmonella persisters12.
No effect of auxotrophy and persisters
To explore further the effect of Salmonella physiology on antibiotic clearance in vivo, we tested two gene alleles reportedly affecting persister formation. First, we examined a hisGP69L allele that repairs the histidine auxotrophy of Salmonella strain SL134438 used throughout this study. Histidine auxotrophy has been suggested to favour antibiotic tolerance over persistence in vivo, where histidine-limiting conditions are assumed to exist39. However, auxotrophic Salmonella SL1344 and prototrophic Salmonella SL1344 hisGP69L have undistinguishable replication dynamics and net growth in mice3, indicating that host tissues supply sufficient histidine to support the biomass needs of SL1344. Auxotrophic Salmonella SL1344 and prototrophic Salmonella SL1344 hisGP69L also exhibited superimposable killing kinetics in enrofloxacin-treated mice (Fig. 1a and Extended Data Fig. 2f; SL1344, survival at 1 h, 5.4 ± 1.8%; 4 h, 2.2 ± 1.2%; SL1344 hisGP69L: 1 h, 4.3 ± 1.1%; 4 h, 1.5 ± 0.4%;). Thus, the histidine auxotrophy of SL1344 does not affect its antibiotic survival in vivo (Supplementary Note 6).
In addition, we tested a variant of the antitoxin ShpB Q97* (ShpB1) that lacks the last four amino acids, which increases persister frequency in Salmonella40. Salmonella hisGP69L shpBQ97* exhibited an unaltered growth rate and enrofloxacin MIC in vitro (Extended Data Fig. 1b, MIC = 0.06 mg l−1) but survived enrofloxacin exposure in vitro around 30-fold better than wild type (Extended Data Fig. 2g). In mice, Salmonella hisGP69L shpBQ97* showed normal fitness (competitive index versus wild type at day 4 post-infection, 0.79 ± 0.3; n = 6; P = 0.12, one-sample t-test of log-transformed data) and had killing kinetics during enrofloxacin exposure that were undistinguishable from wild type (Extended Data Fig. 2f; Supplementary Note 7). Thus, a mutation increasing the frequency of persisters had no detectable impact on antimicrobial survival in vivo, supporting our model that extensive survival of bulk Salmonella minimizes the impact of minor hyper-resilient persister subsets.
In contrast to our findings, it has been reported that infected macrophages trigger Salmonella to express toxin–antitoxin modules that arrest growth in a subset of Salmonella. These non-replicating persisters maintain an active type 3 secretion system 2 (T3SS-2) which is essential for their survival41 and are proposed to cause eradication failures in infected mice receiving daily 300 mg kg−1 enrofloxacin (30- to 60-fold more than recommended42) for 5 days, starting one day after infection17—before disease symptoms appear, which does not reflect typical clinical scenarios (Supplementary Note 8). Some of these data have been difficult to replicate3,18,43, the role of non-mutated toxin–antitoxin modules for persister formation is debatable18,44,45 (Fig. 1c,d), Salmonella does not require T3SS-2 for antibiotic survival in mice12, and the evidence for any Salmonella surviving such excessive enrofloxacin doses is questionable3,12,43 (Supplementary Note 8). Notably, macrophages do not induce a distinct subset of non-replicating Salmonella when infected with homogeneously growing Salmonella in vivo or in vitro (using Salmonella cultured under T3SS-2-inducing conditions to simulate ongoing intracellular replication while preventing rapid macrophage pyroptosis)3. A distinct subset of non-replicating intracellular bacteria, largely incapable of resuming growth after being released from host cells, only emerges when macrophages are infected with stationary-phase Salmonella cultures3,17,41. Stationary cultures are highly heterogeneous46,47, and macrophages may solely amplify this pre-existing heterogeneity. In mice, non-replicating Salmonella are observed in the first two days following infection with 2 × 1010 Salmonella17, a dose >107 times higher than typically encountered in natural human infections48 (Supplementary Note 8). Under more clinically relevant infection and treatment conditions, non-replicating Salmonella are rare and have no detectable role in eradication failures3,12. Instead, slow bacterial clearance results from slowly replicating Salmonella, which respond poorly to antibiotic treatment3,12,49.
Broad post-exposure killing
Our findings with enrofloxacin-treated Salmonella raise concerns about interpreting CFU-based killing assays. To test an unrelated pathogen–antibiotic combination, we imaged gfp-expressing Staphylococcus aureus cells in microfluidic devices during and after exposure to flucloxacillin, a first-line β-lactam antibiotic. S. aureus cells started to release their cytosolic contents—indicating death50—after approximately 1 h exposure to flucloxacillin (Fig. 4a–c and Supplementary Video 4). After 4 h of exposure, 15% remained alive, but killing continued post-exposure for several hours, consistent with the long-lived transpeptidase inhibition of the covalent penicillin-binding protein–β-lactam complexes51. Eventually, only around 0.5% of cells survived and formed microcolonies. The standard CFU plot versus exposure time would suggest monoexponential killing with 30-fold inflated rates compared to actual killing during exposure, which began only after a delay50 (Fig. 4c). Thus, CFU again provided a confounded and misleading readout for antibiotic activity.
a, Snapshots of gfp-expressing S. aureus (inverted fluorescence) before, during and after a 2 h exposure to flucloxacillin (FLX) and switching to antibiotic-free brain–heart infusion (BHI) medium (Supplementary Video 4). Scale bar, 5 μm. b, Surviving fractions of S. aureus after 1 h (left), 2 h (middle) or 4 h (right) exposure to flucloxacillin followed by switching to BHI medium (937, 745 and 599 cells pooled from three independent experiments). A growing colony originating from a single cell is counted as one survivor. Summary data for individual replicates are shown in c. c, Surviving fractions of S. aureus after 1 h, 2 h or 4 h exposure to flucloxacillin and after switching to antibiotic-free BHI medium. Data from three independent experiments (619, 745 and 917 cells). Lines connect the geometric means. Two-way ANOVA for difference between survival at the end of exposure and colony-forming fractions. The arrow depicts the post-exposure loss of viability.
Previous reports indicate that more than 90% of bacteria that survive initial exposure to fluoroquinolones, β-lactams, aminoglycosides, cidal macrolides, nalidixic acid or trimethoprim may die during regrowth on standard agar plates (Supplementary Note 3), consistent with extensively documented post-antibiotic effects of these and other antibiotics52. Specialized regrowth conditions can improve survival by more than 10-fold in most of these cases, but substantial post-exposure death might be unavoidable owing to ongoing damaging effects of remaining target-bound antibiotic (Fig. 3f). As we show here, this post-exposure killing during regrowth can generate artificial biphasic CFU kinetics (Fig. 3d,i), undermining the reliability of the standard persister assay. Additionally, CFU assays may suggest exaggerated killing rates (Figs. 3d,g,i and 4c) and may conflate tolerance (slower killing during exposure) with reduced post-exposure killing (for example, due to slower regrowth; Fig. 3g). Thus, commonly used yet potentially misleading CFU assays should be replaced with real-time, single-cell monitoring of antibiotic action to quantify bacterial killing, tolerance and persistence. For several antibiotic classes, this will require novel reporters for antibiotic-induced damage and viability.
Discussion
Invasive salmonellosis is a life-threatening disease that requires antimicrobial chemotherapy. The recommended bactericidal antibiotics, fluoroquinolones and cephalosporins, achieve only slow Salmonella clearance and are prone to eradication failures, even when the causative Salmonella strain tests as susceptible in the laboratory. This poor efficacy is usually attributed to bacterial stress-induced tolerance and persisters. However, our quantitative comparison under physiological conditions suggests that the main reason is nutrient starvation, which restricts Salmonella replication in infected tissues3,4,5. Salmonella also experiences various stresses in vivo. Although some stresses affect antibiotic survival, their overall effects are limited compared with the dominant role of starvation. Thus, future antibiotic development should mimic nutrient-scarce conditions.
Antimicrobial treatment failures are often attributed to a small subset of non-replicating, hyper-resilient bacteria known as persisters. Persisters are implicated when antibiotic exposure causes an initial rapid decline in CFUs, followed by a slower decrease. Salmonella exhibited such a biphasic CFU decline during enrofloxacin treatment in mice. However, we found that standard CFU assays were misleading because enrofloxacin remains bound to its bacterial target gyrase even after washing, continuing to kill the bacteria during regrowth on the plates, which results in low CFU counts even for short treatment intervals. Similar issues may occur with a wide range of other antibiotics. Thus, CFU-based killing assays can provide confounded and misleading results, suggesting non-existing distinct subsets of bacteria with different susceptibilities, underestimating the number of survivors, and misrepresenting their relationship to the bulk population. Using more appropriate single-cell, real-time assays, we found that damage kinetics were rather uniform across the Salmonella population and much slower than CFU data suggested. More than 35% of Salmonella did not experience any serious damage during 4 h of enrofloxacin exposure, minimizing the influence of rare hyper-resilient persisters. Ceftriaxone also exhibited homogeneously slow killing activity. Thus, the bulk of Salmonella, not just a small subset, were difficult to kill. This was consistent with the slow, steady Salmonella clearance over several days of treatment with no detectable effect of non-replicating persisters3,12.
Our results with two recommended classes of bactericidal antibiotics for treating invasive salmonellosis challenge common assumptions about bacterial resilience and highlight the dominant role of starvation of the entire Salmonella population. The limited effects of stresses and persisters observed in our study are consistent with the broad clinical efficacy of short antibiotic treatments for most infections caused by non-resistant bacteria53, suggesting limited interference from inflammation-associated stresses and persisters. Longer treatment is required for difficult-to-treat infections such as invasive salmonellosis, tuberculosis, deep-seated S. aureus infections and brucellosis. Inefficient drug delivery to infected tissues, biofilms and noncompliant patients may contribute to this problem. These infections also have long incubation periods54,55,56,57, suggesting slow pathogen growth in human tissues. Quantifying the effects of slow growth, stresses and persisters will require real-time, single-cell assays under physiologically relevant conditions.
Methods
Microbiology and molecular biology
Salmonella strains used in this study were based on S. enterica serovar Typhimurium SL1344 hisGL69P xyl38,58. A histidine-prototrophic derivative SL1344 hisGP69L and mutants ΔtisB and ΔecnB ΔshpAB ΔphD-doc have been previously described3. Salmonella lexA3 were generated by generalized transduction using P22 phage JS841 ΔlexA33::[Cm lexA3(Ind−)](sw)59,60. gfp-expressing strains carried gfp.mut2 in the chromosomal sifB locus that has homogenous high activity in vivo38,58. The recAR29A-mCherry DNA damage sensor strain carried a pSC101-derivative with the native PrecA promoter (SL1344 chromosome positions 2,998,612 to 2,998,642) with a modified ribosomal binding site (AGGAA instead of AGGAG) to reduce translation to levels just sufficient for imaging; the entire SL1344 recA gene without stop codon and a change of codon 29 from CGT (encoding arginine) to GCG (encoding alanine)31; a GGGAGCATC linker encoding Gyl-Ser-Ile31; and mCherry without the start ATG. The SOS reporter strain carried mCherry in the chromosomal virK locus61 for detecting all bacteria regardless of their SOS response and a pSC101-derivative with a transcriptional fusion of the SOS-inducible Pcad promoter36 of colicin D62 to gfp-ova coding for a degradable green fluorescent protein variant61 (half-life in the range of 30 min). The Pcad promoter was obtained as synthetic DNA corresponding to bases 6389 to 6675 of pColD-157 (Genbank Y10412.1)63 with base 6621 ‘C’ instead of ‘T’ and base 6628 ‘T’ instead of ‘C’36 followed by TTAAAAGTCAAAGAGGTGTTTTTGC, containing the ribosomal binding site upstream of cda in pColD-CA2336,62. hipA from E. coli BW25113 was mutagenized to obtain hipA D88N and expressed in Salmonella hisGP69L from the constitutive PybaJ promoter64 with a suboptimal ribosomal binding site AAGAG together with PybaJ-timerbac (ref. 3) on a pSC101-derivative. Salmonella hisGP69L shpB1 was constructed by two consecutive single cross-overs65 to change codon 97 from CAA to TAA, resulting in a Q97* mutation, which truncates ShpB by 4 C-terminal amino acids40.
Salmonella was grown in Lennox LB containing 90 mg l−1 streptomycin and 50 mg l−1 kanamycin, or in cation-adjusted Mueller–Hinton broth. To mimic in vivo conditions, we cultured Salmonella in chemostat medium (100 mM MES, 5 mM KCl, 15 mM NH4Cl, 0.5 mM K2SO4, 1 mM KH2PO4, 50 μM MgSO4, 0.02% casamino acids, 0.02% glycerol, 0.0042% N-acetyl-glucosamine, 0.003% glucose, 0.0018% glucosamine, 0.005% histidine, 25 mM NaHCO3, pH 5.5; sterile filtered) with a constant stream of 10% O2/5 % CO2 in mini-chemostats66 at various dilution rates (modifications to these conditions are explained in Fig. 2a). Hydrogen peroxide was added 30 min before antibiotic treatment. Growth conditions were maintained for 72 h before addition of antibiotics. For growth in microfluidics devices, we used the same chemostat medium with 1,000-fold decreased levels of all carbon and energy sources.
To determine killing of diluted batch cultures, we diluted overnight cultures 1:1,000 in fresh pre-warmed medium followed by growth for 3 h before antibiotic treatment. For comparing Salmonella hisGP69L and Salmonella hisGP69L shpBQ97*, we grew day cultures for only 1 h before antibiotic treatment as described40. To minimize experimental variation in these experiments due to undefined stationary cultures, we standardized the preparation of stationary cultures by inoculating primary overnight cultures from 1-day plate cultures, diluting the cultures after overnight growth 1:1,000 in fresh pre-warmed medium, growing these primary day cultures until exponential phase to an OD600 of ~0.2, adjusting them to OD600 = 0.1 followed by dilution 1:1,000 in fresh pre-warmed medium, growth for 14 h (secondary defined overnight culture), diluting them again 1:1,000 in fresh pre-warmed medium and treated them with enrofloxacin 1 h later. To remove antibiotics from dilute cultures with minimal loss of Salmonella during washing, we mixed the bacterial culture with ~109 CFU diaminopimelic acid-dependent E. coli JKe20165. These additional bacteria provided sufficient cell mass for a visible and physically stable cell pellet after centrifugation, permitting recovery of >90% of the surviving Salmonella after two washing steps to remove the antibiotic. Plating of the resuspended pellets on LB plates without diaminopimelic acid enabled growth of Salmonella but not the mixed-in diaminopimelic acid-dependent E. coli strain.
We used S. aureus strain PROSA28, a strain of clonal complex 45 isolated from a patient with an implant-associated joint infection at University Hospital Basel. We transformed this strain with a pRN11-derivative67 carrying a transcriptional fusion of the PpdhABCD promoter and gfp-mut3.1 obtained from plasmid pC183-S368. S. aureus was grown in BHI medium containing 10 mg l−1 chloramphenicol, or in BHI medium diluted 1:50 with saline (for microfluidics experiments).
Mouse infections and tissue collection
All animal experiments were approved (license 2239, Kantonales Veterinäramt Basel) and performed according to local guidelines (Tierschutz-Verordnung, Basel) and the Swiss animal protection law (Tierschutz-Gesetz). We estimated sample size by a sequential statistical design. We first infected two to three mice each based on effect sizes and variation observed in our previous studies5, and used the results to estimate group sizes for obtaining statistical significance with sufficient power.
Female 10- to 16-week-old BALB/c mice (Charles River Laboratories) were infected by tail-vein injection of ~1,000 CFU Salmonella grown to late-log phase in Lennox LB containing 10 mM MgCl2 (which increased consistency across experiments). The inoculum size was determined by plating. Intravenously infected mice show similar Salmonella growth rates3 and Salmonella localization in spleen69 compared to orally infected mice but exhibit less variation in Salmonella tissue loads between individual mice, and thus require fewer experimental animals for detecting differences with the same statistical power. Some mice received at day 5 post-infection an intraperitoneal injection of 5 mg kg−1 enrofloxacin or 50 mg kg−1 ceftriaxone. For plating, mice were euthanized with carbon dioxide and spleen was homogenized in PBS containing 0.2% Triton X-100. Salmonella load was determined by plating. Salmonella survival after enrofloxacin administration was determined by comparing flow cytometry counts and corresponding CFU counts of sorted Salmonella populations as described12. Salmonella survival after ceftriaxone administration was determined by plating.
Randomization
Control and experimental animals were co-housed. We ensured that litter mate or age-matched and healthy animals with identical sex were used in all experiments. In order to reduce the impact of covariates such as housing and litter size, animals were recruited in a partially randomized manner while taking these factors into account. Control and treated animals were infected with the same inoculum to control for bacterial variation. Data derived from animals were pooled by genotype and/or condition after analyses were completed. Comparisons of isogenic Salmonella strains in mice were performed using competitive (mixed) infections to control for variation between experimental animals.
Blinding
Data acquisition for drug treatments could not be blinded because the comparisons were made as pre- versus post-drug treatment, the treatment sequence was essential, and often only one drug was applied. For animal welfare reasons, researchers were not blinded to mouse genotype during study and data collection. Specifically, Slc11a1s mice have to be euthanized at day 4 post-infection to prevent high severity grades, whereas Slc11a1r mice reach similar bacterial loads only at day 6 post-infection. All other data were collected and analysed without blinding but objectively, using instruments without bias and analysis definitions that were uniformly applied to all data sets.
Flow cytometry
Spleen was homogenized in ice-cold PBS containing 0.2% Triton X-100. All samples were kept on ice until analysis. Large host cell fragments were removed by centrifugation at 500g for 5 min. Relevant spectral parameters were recorded in a FACS Fortessa II operated using BD FACSDIVA V8.0.1 software and equipped with 405 nm, 488 nm and 561 nm lasers (Becton Dickinson), using a threshold on side scatter to exclude electronic noise. We used the following channels: GFP and green TIMER component, excitation 488 nm, emission 502–525 nm; mCherry and orange TIMER component, excitation 561 nm, emission 595–654 nm with red laser (633 nm) switched off; red autofluorescence channel, excitation 488 nm, emission 663–677 nm (the gating strategy for mCherry-Salmonella is shown in Extended Data Fig. 2c). Salmonella cells were purified from infected spleen homogenates using an Aria IIIu cell sorter (BD Biosciences) using excitation 488 nm and emission channels 499–529 nm (predominantly GFP) and 573–613 (predominantly host autofluorescence) as well as excitation 561 nm and emission 595–617 nm. Defined sample volumes of the sorted Salmonella were re-analysed by flow cytometry and plating to determine survival rates12. Data were processed with FlowJo 10.6.1 and further analysed with OriginPro 2019 (64-bit) 9.6.0.172.
Microfluidics experiments
Salmonella expressing recAR29A-mCherry were grown overnight in chemostat medium, diluted 1:50 in chemostat medium with 100-fold decreased concentrations of carbon and energy sources, grown for 6 h, inoculated in CellASIC ONIX B04A-03 microfluidic plates (Millipore) operated in a CellASIC ONIX Microfluidic System, and grown for 6 h in chemostat medium with 1,000-decreased concentrations of carbon/energy sources (generation time ~3 h), before exposing them to enrofloxacin in the same medium. After various time intervals bacteria were switched back to chemostat medium with 1,000-fold decreased concentrations of carbon/energy sources, and to Lennox lysogeny broth. gfp-expressing S. aureus were grown overnight in BHI medium diluted 1:50 with saline, diluted 1:50 in fresh medium, grown for 4 h, and inoculated in the microfluidic plates. After growth for 4 h in 1:50 BHI (generation time ~1.5 h), bacteria were exposed to various time intervals to 12 mg l−1 flucloxacillin in the same medium, and then switched to normal BHI.
Bacteria were imaged using a Nikon Eclipse Ti2 inverted microscope equipped with Perfect Focus System and Plan Apo 100× Oil Ph3 DM (NA 1.45) objective lens (MRD31905), SPECTRA X light engine (Lumencor), phase contrast (8% light intensity, 200 ms exposure) and a Dualband EGFP/mCherry filter set (Chroma 59022 ET; for S. aureus, 470 nm excitation, 4% light intensity, 150 ms exposure; for Salmonella, 575 nm excitation, 5% light intensity, 250 ms exposure), a Hamamatsu ORCA-Flash4.0 V3 CMOS camera (C13440-20CU) with pixel size of 65 nm, and NIS-Elements (Nikon). Images were acquired at 1 min (Salmonella) or 5 min (S. aureus) intervals at 37 °C with 95% humidity controlled by Okolab T-unit (Okolab). Images were analysed with ImageJ 1.53q70 using plugins MultiStackReg71 and FeatureJ-Laplacian (Smoothing scale 2.0) (developed by E. Meijering).
The decay of undamaged cells in Fig. 3i appeared to occur in three stages based on discontinuities in the first derivative of log-transformed data. We fitted each stage separately with monoexponential decays using GraphPad Prism 9.3.1. Data were further analysed with OriginPro 2019 (64-bit) 9.6.0.172.
Statistics
Statistical tests were performed with GraphPad Prism 9.3.1 as indicated in the figure legends. We always used two-tailed tests because we were interested to also test for effects that go into the opposite direction to what we might have predicted. CFU counts approximate normal distributions after log transformation72, thus permitting parametric test statistics. Multiple linear regression was carried out after log-transforming values for dependent and independent variables (except for pH).
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
Data points generated for this study are included in the figures whenever possible. Tabulated data for all figures, videos of the microfluidics experiments and flow cytometry data are available at https://www.ebi.ac.uk/biostudies/studies/S-BSST1727. Source data are provided with this paper.
References
Bjarnsholt, T. et al. The importance of understanding the infectious microenvironment. Lancet Infect. Dis. 22, e88–e92 (2022).
Balaban, N. Q. et al. Definitions and guidelines for research on antibiotic persistence. Nat. Rev. Microbiol. 17, 441–448 (2019).
Claudi, B. et al. Phenotypic variation of Salmonella in host tissues delays eradication by antimicrobial chemotherapy. Cell 158, 722–733 (2014).
Cunrath, O. & Bumann, D. Host resistance factor SLC11A1 restricts Salmonella growth through magnesium deprivation. Science 366, 995–999 (2019).
Steeb, B. et al. Parallel exploitation of diverse host nutrients enhances Salmonella virulence. PLoS Pathog. 9, e1003301 (2013).
Doern, G. V. & Brecher, S. M. The clinical predictive value (or lack thereof) of the results of in vitro. J. Clin. Microbiol. 49, S11–S14 (2011).
WHO Bacterial Priority Pathogens List, 2024: Bacterial Pathogens of Public Health Importance, to Guide Research, Development and Strategies to Prevent and Control Antimicrobial Resistance (World Health Organization, 2024).
Newson, J. P., Gaissmaier, M. S., McHugh, S. C. & Hardt, W. D. Studying antibiotic persistence in vivo using the model organism Salmonella Typhimurium. Curr. Opin. Microbiol. 70, 102224 (2022).
Bumann, D. Heterogeneous host-pathogen encounters: act locally, think globally. Cell Host Microbe 17, 13–19 (2015).
Fang, F. C., Frawley, E. R., Tapscott, T. & Vazquez-Torres, A. Bacterial stress responses during host infection. Cell Host Microbe 20, 133–143 (2016).
Liu, X. et al. Pharmacokinetics and pharmacodynamics of enrofloxacin treatment of Escherichia coli in a murine thigh infection modeling. BMC Vet. Res. 17, 212 (2021).
Li, J. et al. Tissue compartmentalization enables Salmonella persistence during chemotherapy. Proc. Natl Acad. Sci. USA 118, e2113951118 (2021).
Dobinson, H. C. et al. Evaluation of the clinical and microbiological response to Salmonella Paratyphi A infection in the first paratyphoid human challenge model. Clin. Infect. Dis. 64, 1066–1073 (2017).
Wang, E., Bergeron, Y. & Bergeron, M. G. Ceftriaxone pharmacokinetics in interleukin-10-treated murine pneumococcal pneumonia. J. Antimicrob. Chemother. 55, 721–726 (2005).
Dorr, T., Lewis, K. & Vulic, M. SOS response induces persistence to fluoroquinolones in Escherichia coli. PLoS Genet. 5, e1000760 (2009).
Dorr, T., Vulic, M. & Lewis, K. Ciprofloxacin causes persister formation by inducing the TisB toxin in Escherichia coli. PLoS Biol. 8, e1000317 (2010).
Helaine, S. et al. Internalization of Salmonella by macrophages induces formation of nonreplicating persisters. Science 343, 204–208 (2014).
Pontes, M. H. & Groisman, E. A. Slow growth determines nonheritable antibiotic resistance in Salmonella enterica. Sci. Signal. 12, eaax3938 (2019).
Chen, S. et al. Contribution of target gene mutations and efflux to decreased susceptibility of Salmonella enterica serovar typhimurium to fluoroquinolones and other antimicrobials. Antimicrob. Agents Chemother. 51, 535–542 (2007).
Bergmiller, T. et al. Biased partitioning of the multidrug efflux pump AcrAB–TolC underlies long-lived phenotypic heterogeneity. Science 356, 311–315 (2017).
Aldridge, B. B. et al. Asymmetry and aging of mycobacterial cells lead to variable growth and antibiotic susceptibility. Science 335, 100–104 (2012).
Kaldalu, N. & Tenson, T. Slow growth causes bacterial persistence. Sci. Signal. 12, eaay1167 (2019).
Rotem, E. et al. Regulation of phenotypic variability by a threshold-based mechanism underlies bacterial persistence. Proc. Natl Acad. Sci. USA 107, 12541–12546 (2010).
Korch, S. B., Henderson, T. A. & Hill, T. M. Characterization of the hipA7 allele of Escherichia coli and evidence that high persistence is governed by (p)ppGpp synthesis. Mol. Microbiol. 50, 1199–1213 (2003).
Lopatkin, A. J. et al. Bacterial metabolic state more accurately predicts antibiotic lethality than growth rate. Nat. Microbiol. 4, 2109–2117 (2019).
Tuomanen, E., Cozens, R., Tosch, W., Zak, O. & Tomasz, A. The rate of killing of Escherichia coli by beta-lactam antibiotics is strictly proportional to the rate of bacterial growth. J. Gen. Microbiol. 132, 1297–1304 (1986).
Aldred, K. J., Kerns, R. J. & Osheroff, N. Mechanism of quinolone action and resistance. Biochemistry 53, 1565–1574 (2014).
Wiktor, J. et al. RecA finds homologous DNA by reduced dimensionality search. Nature 597, 426–429 (2021).
Amarh, V., White, M. A. & Leach, D. R. F. Dynamics of RecA-mediated repair of replication-dependent DNA breaks. J. Cell Biol. 217, 2299–2307 (2018).
Lesterlin, C., Ball, G., Schermelleh, L. & Sherratt, D. J. RecA bundles mediate homology pairing between distant sisters during DNA break repair. Nature 506, 249–253 (2014).
Renzette, N. et al. Localization of RecA in Escherichia coli K-12 using RecA-GFP. Mol. Microbiol. 57, 1074–1085 (2005).
Azevedo, N. F. et al. Proposal for a method to estimate nutrient shock effects in bacteria. BMC Res. Notes 5, 422 (2012).
Wiedemann, B. & Kratz, B. in Ciprofloxacin iv. Defining its Role in Serious Infection (ed. Garrard, C.) 13–19 (Springer, 1993).
Mok, W. W. K. & Brynildsen, M. P. Timing of DNA damage responses impacts persistence to fluoroquinolones. Proc. Natl Acad. Sci. USA 115, E6301–e6309 (2018).
Pontes, M. H. & Groisman, E. A. A physiological basis for nonheritable antibiotic resistance. mBio 11, e00817–e00820 (2020).
Norman, A., Hestbjerg Hansen, L. & Sorensen, S. J. Construction of a ColD cda promoter-based SOS–green fluorescent protein whole-cell biosensor with higher sensitivity toward genotoxic compounds than constructs based on recA, umuDC, or sulA promoters. Appl. Environ. Microbiol. 71, 2338–2346 (2005).
Malik, M., Hussain, S. & Drlica, K. Effect of anaerobic growth on quinolone lethality with Escherichia coli. Antimicrob. Agents Chemother. 51, 28–34 (2007).
Hoiseth, S. K. & Stocker, B. A. Aromatic-dependent Salmonella typhimurium are non-virulent and effective as live vaccines. Nature 291, 238–239 (1981).
Michaux, C., Ronneau, S., Giorgio, R. T. & Helaine, S. Antibiotic tolerance and persistence have distinct fitness trade-offs. PLoS Pathog. 18, e1010963 (2022).
Slattery, A., Victorsen, A. H., Brown, A., Hillman, K. & Phillips, G. J. Isolation of highly persistent mutants of Salmonella enterica serovar typhimurium reveals a new toxin–antitoxin module. J. Bacteriol. 195, 647–657 (2013).
Stapels, D. A. C. et al. Salmonella persisters undermine host immune defenses during antibiotic treatment. Science 362, 1156–1160 (2018).
Slate, A. R. et al. Efficacy of enrofloxacin in a mouse model of sepsis. J. Am. Assoc. Lab. Anim. Sci. 53, 381–386 (2014).
Griffin, A. J., Li, L. X., Voedisch, S., Pabst, O. & McSorley, S. J. Dissemination of persistent intestinal bacteria via the mesenteric lymph nodes causes typhoid relapse. Infect. Immun. 79, 1479–1488 (2011).
Jurėnas, D., Fraikin, N., Goormaghtigh, F. & Van Melderen, L. Biology and evolution of bacterial toxin–antitoxin systems. Nat. Rev. Microbiol. 20, 335–350 (2022).
LeRoux, M. & Laub, M. T. Toxin–antitoxin systems as phage defense elements. Annu. Rev. Microbiol. 76, 21–43 (2022).
Ryall, B., Eydallin, G. & Ferenci, T. Culture history and population heterogeneity as determinants of bacterial adaptation: the adaptomics of a single environmental transition. Microbiol. Mol. Biol. Rev. 76, 597–625 (2012).
Ciolli Mattioli, C. et al. Physiological stress drives the emergence of a Salmonella subpopulation through ribosomal RNA regulation. Curr. Biol. 33, 4880–4892.e14 (2023).
Woodward, W. E. Volunteer studies of typhoid fever and vaccines. Trans. R. Soc. Trop. Med. Hyg. 74, 553–556 (1980).
Kaiser, P. et al. Cecum lymph node dendritic cells harbor slow-growing bacteria phenotypically tolerant to antibiotic treatment. PLoS Biol. 12, e1001793 (2014).
Giesbrecht, P., Kersten, T., Maidhof, H. & Wecke, J. Staphylococcal cell wall: morphogenesis and fatal variations in the presence of penicillin. Microbiol. Mol. Biol. Rev. 62, 1371–1414 (1998).
Davoodi, S., Daryaee, F., Chang, A., Walker, S. G. & Tonge, P. J. Correlating drug-target residence time and post-antibiotic effect: insight into target vulnerability. ACS Infect. Dis. 6, 629–636 (2020).
MacKenzie, F. M. & Gould, I. M. The post-antibiotic effect. J. Antimicrob. Chemother. 32, 519–537 (1993).
Grant, J. & Saux, N. L. Duration of antibiotic therapy for common infections. J. Assoc. Med. Microbiol. Infect. Dis. Can. 6, 181–197 (2021).
Awofisayo-Okuyelu, A., McCarthy, N., Mgbakor, I. & Hall, I. Incubation period of typhoidal salmonellosis: a systematic review and meta-analysis of outbreaks and experimental studies occurring over the last century. BMC Infect. Dis. 18, 483 (2018).
Behr, M. A., Edelstein, P. H. & Ramakrishnan, L. Revisiting the timetable of tuberculosis. BMJ 362, k2738 (2018).
Smit, J. et al. Onset of symptoms, diagnostic confirmation, and occurrence of multiple infective foci in patients with Staphylococcus aureus bloodstream infection: a look into the order of events and potential clinical implications. Infection 46, 651–658 (2018).
Hasanjani Roushan, M. R. & Ebrahimpour, S. Human brucellosis: an overview. Caspian J. Intern. Med. 6, 46–47 (2015).
Kroger, C. et al. The transcriptional landscape and small RNAs of Salmonella enterica serovar Typhimurium. Proc. Natl Acad. Sci. USA 109, E1277–E1286 (2012).
Bunny, K., Liu, J. & Roth, J. Phenotypes of lexA mutations in Salmonella enterica: evidence for a lethal lexA null phenotype due to the Fels-2 prophage. J. Bacteriol. 184, 6235–6249 (2002).
Craig, M. & Slauch, J. M. Phagocytic superoxide specifically damages an extracytoplasmic target to inhibit or kill Salmonella. PLoS ONE 4, e4975 (2009).
Rollenhagen, C., Sorensen, M., Rizos, K., Hurvitz, R. & Bumann, D. Antigen selection based on expression levels during infection facilitates vaccine development for an intracellular pathogen. Proc. Natl Acad. Sci. USA 101, 8739–8744 (2004).
Roos, U., Harkness, R. E. & Braun, V. Assembly of colicin genes from a few DNA fragments. Nucleotide sequence of colicin D. Mol. Microbiol. 3, 891–902 (1989).
Hofinger, C., Karch, H. & Schmidt, H. Structure and function of plasmid pColD157 of enterohemorrhagic Escherichia coli O157 and its distribution among strains from patients with diarrhea and hemolytic–uremic syndrome. J. Clin. Microbiol. 36, 24–29 (1998).
Rollenhagen, C. & Bumann, D. Salmonella enterica highly expressed genes are disease specific. Infect. Immun. 74, 1649–1660 (2006).
Cianfanelli, F. R., Cunrath, O. & Bumann, D. Efficient dual-negative selection for bacterial genome editing. BMC Microbiol. 20, 129 (2020).
Nanchen, A., Schicker, A. & Sauer, U. Nonlinear dependency of intracellular fluxes on growth rate in miniaturized continuous cultures of Escherichia coli. Appl. Environ. Microbiol. 72, 1164–1172 (2006).
de Jong, N. W., van der Horst, T., van Strijp, J. A. & Nijland, R. Fluorescent reporters for markerless genomic integration in Staphylococcus aureus. Sci. Rep. 7, 43889 (2017).
Burian, M. et al. Temporal expression of adhesion factors and activity of global regulators during establishment of Staphylococcus aureus nasal colonization. J. Infect. Dis. 201, 1414–1421 (2010).
Burton, N. A. et al. Disparate impact of oxidative host defenses determines the fate of Salmonella during systemic infection in mice. Cell Host Microbe 15, 72–83 (2014).
Schneider, C. A., Rasband, W. S. & Eliceiri, K. W. NIH Image to ImageJ: 25 years of image analysis. Nat. Methods 9, 671–675 (2012).
Thévenaz, P., Ruttimann, U. E. & Unser, M. A pyramid approach to subpixel registration based on intensity. IEEE Trans. Image Process. 7, 27–41 (1998).
Becker, D. et al. Robust Salmonella metabolism limits possibilities for new antimicrobials. Nature 440, 303–307 (2006).
Volkmer, B. & Heinemann, M. Condition-dependent cell volume and concentration of Escherichia coli to facilitate data conversion for systems biology modeling. PLoS ONE 6, e23126 (2011).
Acknowledgements
The authors thank J. Slauch for the lexA3 phage lysate; R. Kühl and N. Khanna for strain S. aureus PROSA28; R. Nijland for plasmid pRN11; A. Peschel for plasmid pC183-S3; and M. Basler, U. Jenal, R. Kühl, C. Dehio, M. Zampieri, T. Tenson, N. Kaldalu and M. Putrinš for helpful discussions. D.B. received support from Schweizerischer Nationalfonds (51NF40_180541 NCCR AntiResist, 310030_156818 and NRP 72−177449).
Funding
Open access funding provided by University of Basel.
Author information
Authors and Affiliations
Contributions
Experiments were conceived and designed by J.F., V.T., F.G. and D.B. Chemostat and batch culture experiments were performed and analysed by J.F. and B.C. Mouse infections were carried out and analysed by B.C. and J.L. Microfluidics experiments were done by V.T. and F.G. and analysed by V.T. and D.B. Figure design, manuscript writing and editing were carried out by D.B. with input from all authors. Project supervision and funding were undertaken by D.B.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature thanks the anonymous reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data figures and tables
Extended Data Fig. 1 Analysis of Salmonella in vitro.
(a) Sorting of Salmonella cells with different sizes. Salmonella expressing gfp under control of the chromosomal PsifB promoter61 showed correlated sideward-scatter (a proxy for size73) and green fluorescence signals. The combination of the two detection channels increased resolution and enabled enrichment of subsets by flow cytometric sorting using the gate boundaries shown as dashed red lines. (b) Growth curves in lysogeny broth in 96-well plates. Means and SDs for 4 (wild-type, WT), 5 (hipAD88N), or 6 (shpBQ97*) biological replicates (each measured in technical triplicates) are shown (OD600, optical density at 600 nm; Det. Lim., detection limit). (c) Division rate distributions of Salmonella strains in different mouse genotypes (data for wild-type Salmonella in SLC11A1r mice from4, n = 61,137 cells from seven independently infected mice; SLC11A1s, WT n = 34,851 from three independently infected mice; SLC11A1s, hipAD88N n = 832 from three independently infected mice). The inset shows medians for the individual mice (SLC11A1s WT/hipAD88N n = 3; SLC11A1r, WT n = 7; ANOVA with comparison against SLC11A1s, WT; P-values adjusted for multiple comparisons according to Holm-Šídák). (d) Survival of Salmonella strains in mouse spleen 1 h after administration of 0.1 mg enrofloxacin. Each circle represents an individual mouse (SLC11A1s: WT n = 10; hipAD88N n = 4; SLC11A1r, WT n = 7) two-tailed t-test, P-values adjusted for multiple comparisons according to Holm-Šídák). (e) Analysis of Salmonella/pRecA-mCherry fluorescence images. Detection of RecA-mCherry foci was enhanced by 2D Laplacian of Gaussian filtering (approximating a second derivative) of red fluorescence and false-color visualization. (f) Fraction of cells with no long-lasting RecA focus (“undamaged fraction”) during growth without enrofloxacin (Control, 146 cells), or exposure from t = 0 h to 1.5 or 5 mg/L enrofloxacin (130, 250 cells). The dotted lines represent monoexponential fits. The data for 5 mg/L are also shown in Fig. 3c. Summary data for the 5 mg/L exposure and an independent replicate are shown in Fig. 3d. (g) Flow-cytometry analysis of sideward scatter as a read-out for cell size73 of Salmonella before and after 1 h exposure to enrofloxacin during exponential growth in lysogeny broth (LB), slow growth in tissue-mimicking chemostats, or in mouse spleen. Each symbol represents an independent culture or an individual mouse (LB +/− n = 3; Chemostat +/− n = 5; Mouse spleen +/− n = 3; two-tailed t-test of log-transformed data with Holm-Šídák correction for multiple comparisons). (h) Snap-shots of Salmonella growing in nutrient-poor minimal medium (MM) without enrofloxacin and then in lysogeny broth (LB; video S1). (i) Fraction of undamaged cells before and after switching to LB, and dividing Salmonella after the LB switch (146 cells; LoD, limit of detection). RecA foci during the first 4 h are also shown in panel f (‘Control’). The dotted line is a monoexponential fit for damage before the LB switch. (j) Time difference between detection of a DNA double-strand bread (DSB) based on a long-lasting RecA focus, and re-initiation of cell division. Control cells without enrofloxacin exposure that were switched to lysogeny broth (No ENR/LB: DSB- n = 40; DSB+ n = 69), cells exposed for 1 h to enrofloxacin followed by a switch to LB (1 h/LB n = 35), and cells exposed to declining concentrations of enrofloxacin over 7 h followed by continuing incubation in nutrient-poor medium (‘in vivo-mimicking’, IVM n = 115) are shown. Each circle represents an individual cell. The statistical difference between groups was test using the Kruskal-Wallis-test with Dunn’s correction for multiple testing.
Extended Data Fig. 2 Salmonella analysis in vivo.
(a) Traditional model and actual mechanism underlying rapid loss of colony-forming units. In the traditional models, a small subset of persisters, some of which are triggered by stresses, survive antibiotic exposure and give rise to colonies on plates. However, antibiotic exposure actually kills only few cells, but survivors are poisoned by drug, which remains bound to its target (depicted as yellow symbols). Most of these poisoned cells die after plating. Thus, colony counts reflect mostly post-exposure killing rather than viability loss during exposure. (b) Plasmid map of the SOS-reporter construct. The Pcad promoter is repressed by LexA36. LexA self-cleavage (SOS-response) is associated with unbinding of LexA to DNA, de-repressing Pcad. gfp-ova encodes a destabilized GFP variant to report current promoter activities. aphA encodes aminoglycoside phosphotransferase conferring resistance to kanamycin. repA encodes RepA which replicates plasmids with a oriSC101 origin (T, terminator). (c) Gating strategy for identifying Salmonella reporter cells in spleen homogenates based on the red fluorescence of chromosomally encoded mCherry (Ex, excitation wavelength; Em, emission range). mCherry-Salmonella were then analyzed for green fluorescence as shown in Fig. 3h. (d) Green fluorescence of Salmonella retrieved from mouse spleen 4 h after enrofloxacin administration and incubated for 3 h in lysogeny broth (LB). Control Salmonella without gfp are also shown. The data represent histograms pooled from 2 mice. (e) Colony recovery of GFP− (SOS−) and GFP+ (SOS+) Salmonella sorted from spleen homogenates from untreated mice (0 h), or from treated mice 1 h or 4 h after enrofloxacin administration. Survival was determined by plating on lysogeny-broth plates. Each circle represents an individual mouse (untreated n = 14; 1 h GFP +/− n = 6; 4 h GFP +/− n = 4). The statistical difference of GFP- and GFP+ contributions from treated mice was tested by two-way ANOVA (column factor, two-tailed, single comparison). (f) Survival of Salmonella strains in enrofloxacin-treated mice (hisGP69L: 1 h n = 10; 4 h n = 6; hisGP69L shpBQ97* 1 h/4 h n = 3; geometric means and geometric SDs; two-way ANOVA of log-transformed data). (g) Survival of Salmonella strains in lysogeny broth with enrofloxacin (geometric means and geometric SDs; six independent cultures from two different experiments; two-way ANOVA of log-transformed data).
Supplementary information
Supplementary Notes
Eight supplementary notes that describe previously published data and their contributions to the analyses provided in the main text.
Supplementary Video 1
Responses of Salmonella to a switch to LB medium. Formation of RecA foci in Salmonella growing in nutrient-poor medium that were subsequently shifted to rich lysogeny broth.
Supplementary Video 2
Responses of enrofloxacin-treated Salmonella to a switch to LB medium. Formation of RecA foci and induction of SOS responses in Salmonella growing in nutrient-poor medium that were exposed to enrofloxacin for 4 h and subsequently shifted to rich lysogeny broth.
Supplementary Video 3
Responses of enrofloxacin-treated Salmonella in nutrient-poor medium. Formation of RecA foci and induction of SOS responses in Salmonella growing in nutrient-poor medium that were exposed to declining concentrations of enrofloxacin for 7 h and subsequently maintained in nutrient-poor medium.
Supplementary Video 4
Responses of flucloxacillin-treated S. aureus. Loss of cytosolic green fluorescent protein in S. aureus growing in nutrient-poor medium that were exposed to flucloxacillin and subsequently shifted to nutrient-rich brain–heart infusion.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fanous, J., Claudi, B., Tripathi, V. et al. Limited impact of Salmonella stress and persisters on antibiotic clearance. Nature 639, 181–189 (2025). https://doi.org/10.1038/s41586-024-08506-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41586-024-08506-6