Research news
Trial of engasertib AKT inhibitor reduces nosebleeds in rare hereditary disorder
Dec 03 2025
A placebo-controlled trial has shown that the oral AKT inhibitor engasertib could reduce the frequency and duration of nosebleeds in people with the rare vascular disorder hereditary haemorrhagic telangiectasia
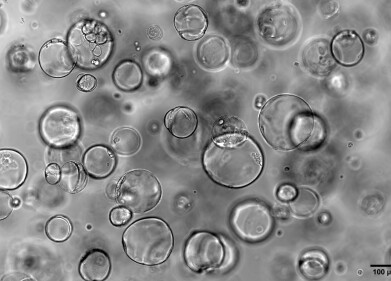
Hereditary haemorrhagic telangiectasia (HHT), an inherited vascular disorder that causes fragile and abnormal blood vessels, is the second most common inherited bleeding disorder worldwide and affects about 1 in 3,800 people. While the condition often first presents with chronic, spontaneous nosebleeds it can also involve internal bleeding and arteriovenous malformations in vital organs such as the lungs, liver and brain impairment to quality of life and lower life expectancy.
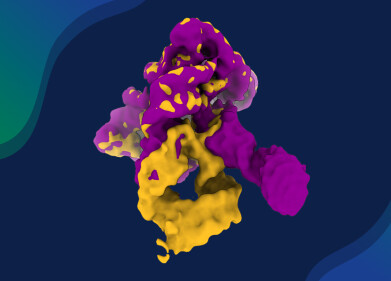
In HHT, pathogenic variants disrupt the activin receptor like kinase 1 (ALK1) pathway, which normally helps to regulate the formation and maintenance of blood vessels. This disruption leads to excessive activation of AKT, a serine/threonine protein kinase that promotes cell survival and vessel growth. Engasertib is an oral, once-daily small-molecule inhibitor of AKT that has been developed by Vaderis Therapeutics to specifically target this dysregulated signalling pathway in HHT.
A recent double-blind, randomised, placebo-controlled study at Mass General Brigham, Boston, Massachusetts, has evaluated the safety and efficacy of engasertib in adults with HHT who experienced clinically significant epistaxis. The trial enrolled 75 participants, who were randomly assigned to receive 30 milligrams of engasertib, 40 milligrams of engasertib, or a placebo once daily for 12 weeks.
The primary focus was safety and tolerability, together with the effect of engasertib on the frequency and duration of nosebleeds, which represent a major day-to-day burden for patients with HHT. At baseline, participants often experienced multiple nosebleeds per week and many had a long history of iron deficiency anaemia, blood transfusions or prior invasive procedures to control bleeding.
“HHT causes serious vascular abnormalities throughout the body, often to lead to dangerous, abnormal blood vessels in the brain, lungs and liver, which bring with them major complications including stroke, heart failure and brain haemorrhage, yet a licensed treatment does not exist,” said co-lead principal investigator and first author Dr. Hanny Al-Samkari, a haematologist at Mass General Brigham and co-director of the Hereditary Haemorrhagic Telangiectasia Center of Excellence at Massachusetts General Hospital.
“This engasertib trial is a step toward a better life for these patients, and I am thrilled we found it to be both safe and effective at decreasing bleeding in HHT,” he added.
After 12 weeks of treatment, participants who received engasertib had fewer and shorter nosebleeds than those who had been given the placebo. And the benefit received appeared to be dose related. In the 40 milligram group, 61 per cent of participants reported that they felt ‘much better’ at the end of the study, compared with 37 per cent in the 30 milligram group and 27 per cent in the placebo group.
These subjective reports aligned with diary-based measures of epistaxis burden, which indicated a reduction in both the frequency of episodes and their average duration among those who received active treatment.
The safety profile of engasertib was also favourable within the 12-week trial period. The investigators judged the drug to be safe in this cohort. The most common adverse effect was a mild but reversible skin rash which tended to resolve without the need to stop treatment. The rate of serious adverse events did not significantly differ between the engasertib and placebo groups which supports the feasibility of longer-term studies in broader patient populations.
The absence of an approved therapy for HHT from any major regulatory body worldwide – including the FDA, MHRA, EMA, Australia’s TGA and Health Canada – has left clinicians to rely on supportive care, such as iron supplementation, blood transfusions, local cauterisation or embolisation procedures and off-label use of systemic agents that were not developed for the disorder.
These approaches can control symptoms in some patients but often fail to address the underlying vascular pathology and can carry significant risks. In this context, a targeted oral agent that interferes directly with AKT signalling represents a potentially important shift in the therapeutic landscape.
The authors stressed that the current study was relatively small and only ran for 12 weeks, so it cannot fully define the long-term efficacy or safety of chronic AKT inhibition in HHT. Longer and larger studies will be needed to examine considerations such as the durability of the effect on nosebleeds, its impact on iron status and transfusion requirements, and also to explore if engasertib can also modify internal vascular lesions of organs or reduce the risk of severe complications such as stroke and heart failure.
However, this trial did provide proof of concept that selective AKT inhibition can safely reduce bleeding in HHT. For a rare disorder that has historically lacked any specific, regulator-approved treatment option, engasertib is a promising candidate to move on from early-phase evaluation.
For further reading please visit: 10.1056/NEJMoa2504411
Digital Edition
Lab Asia Dec 2025
December 2025
Chromatography Articles- Cutting-edge sample preparation tools help laboratories to stay ahead of the curveMass Spectrometry & Spectroscopy Articles- Unlocking the complexity of metabolomics: Pushi...
View all digital editions
Events
Jan 21 2026 Tokyo, Japan
Jan 28 2026 Tokyo, Japan
Jan 29 2026 New Delhi, India
Feb 07 2026 Boston, MA, USA
Asia Pharma Expo/Asia Lab Expo
Feb 12 2026 Dhaka, Bangladesh