Microscopy & Microtechniques
How Does Cancer Modelling Assist Treatment?
Nov 07 2021
Each year, almost 10 million people around the world lose their lives prematurely to cancer. In the UK, one in two adults will contract cancer at some point in their lives. Significant investment has gone into cancer research, throwing up some valuable breakthroughs but presenting difficult challenges, as well. While advances in medicine and treatment have advanced to the point that around 50% of patients now go on to live for 10 years or more after their diagnosis, there is still much that remains a mystery around this deadly disease.
Catching tumours early on in their development is crucial to overcoming cancer – but so too is creating a personalised treatment plan tailored to the individual in question. This is because each cancer has different genetic characteristics, which can evolve over time within the environment of the host human. As such, advanced technological techniques are required to assess the specific characteristics of the cancer in question and monitor its development within the patient’s body. Cancer modelling is one such technique.
What is cancer modelling?
Historically, all research into understanding and overcoming cancer took place either in vivo (in a living being, most commonly a laboratory mouse or a human patient) or in vitro (in the laboratory). Both of these options are still pursued in cancer modelling today, with the most common forms of modelling involving the extraction of cancerous tissue from a patient, followed by its study in the lab (in vitro) or in an immunodeficient mouse (in vivo) after injection.
However, the rapid advance of technology in the last few decades has presented a new option: in silico. This revolutionary technique enlists the help of computer programming to envisage how cancers might behave in a virtual setting. This is especially useful in today’s modern age of data collection and storage; with so much information amassed over countless cases and decades of research at our fingertips, scientists have a treasure trove of statistics to base their studies upon. Big data, in particular, has been helpful with this avenue of research.
What is big data?
Big data is the name given to extremely large collections of data, which can be pored over and analysed by computers far more effectively than by humans. Because of the sheer breadth and depth of information available, it can be difficult (if not impossible) for the human brain to ascertain patterns, trends and correlated links within the data – but thanks to the advent of artificial intelligence (AI) and machine learning, computers can now succeed where humans have failed.
This kind of technology is already employed in many aspects of our daily lives, including in the home and workplace. For example, IoT sensors can detect when our fridge is running low on supplies and automatically order replacements, or else remotely adjust temperature and humidity settings in an office to maximise comfort and minimise energy consumption. Big data is also now proving its worth in the medical world via a variety of different applications and disciplines. Cancer modelling is one area where it holds considerable potential.
What are the different types of cancer modelling?
As mentioned above, cancer modelling predates in silico experiments by some distance. In fact, cancer modelling research has taken place for almost two centuries in some form or other! Today, however, there are a wide array of different types of cancer modelling, each of which operates via different methods and has different objectives in mind. Here are some of the most common:
- Tumour growth modelling
There is a wealth of evidence demonstrating how cancer can evolve over time – and how this development can take different forms depending on the environment in which it is growing. For that reason, it’s extremely challenging for doctors to prescribe treatment, since one cancer may behave in a different way from another and even the same one may have evolved by the time the prognosis has been put into action. Tumour growth modelling, therefore, can be helpful in anticipating how a cancer might spread, but can be limited in its non-targeted approach.
- CCL modelling
As science has progressed through the ages, our ability to extract living tissue from a cancer patient has opened up new possibilities in studying the disease. Cancer cell lines (CCLs) which have been taken from a tumour have traditionally been the most common form of obtaining and analysing this information. After extraction, the CCLs are passaged in the laboratory and injected into immunodeficient mice to create xenograft models. While this method has uncovered some important findings about cancer, it has several drawbacks, the most significant of which is that it does not reflect the tumour heterogeneity with adequate accuracy, since it cannot account for the exact environment of the human body.
- PDX modelling
Patient-derived xenograft (PDX) modelling is a relatively new answer to those issues. This technique operates on the same principles as CCL modelling, but attempts to retain as much of the patient’s physiological characteristics as possible by injecting the sample tissue into the mice immediately. With a more faithful representation of the fibroblast, immune cells and vessel cells surrounding the tumour, the researchers are able to see how the cancer develops in an environment that more closely resembles that of the patient. For that reason, it is believed to be more helpful in delivering personalised treatment for the particular individual in question.
Although each of these cancer modelling techniques has advanced our understanding of how cancer operates in the human body, none of them are without drawbacks. Even PDX modelling, the most advanced of the trio, carries an expensive price tag and questions over animal rights with regard to the lab mice involved in experiments. What’s more, extracting the cancerous tissue in this manner only allows scientists a snapshot of the tumour’s behaviour at a precise point in time; by the time a prognosis has been developed, it’s possible the cancer could have again evolved within the patient’s body.
How can microchip technology help?
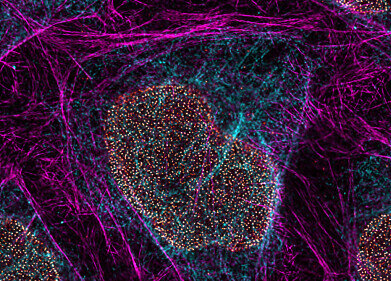
Fortunately, technology has once again lent a helping hand with regard to those issues, this time in the shape of microchips. So-called ‘cancer on a chip’ modelling involves the structuring of the physiology and functions of the affected organ on a microchip, thus recreating an environment very similar to that within the human body. While it would be impossible to replicate the complexity of the body in minute detail, the major physiological elements can be reconstructed satisfactorily.
Into this facsimile of the patient, a sample of their DNA (with the cancerous cells) is theninjected. This approach allows the scientists to witness the development of the tumour in real-time, since it can be monitored continuously (rather than just via the snapshot mentioned above). This should, in theory, give a more accurate reflection of the cancer’s evolution and allow doctors to tailor treatment more appropriately. It is also more cost-effective, less invasive and neatly sidesteps the controversial issues of animal cruelty that so often plague medical research.
How else can cancer modelling help patients?
Besides contributing towards personalised treatment plans that give patients the best chance of overcoming the disease, there are a number of other ways in which cancer modelling can help them. One of these is by monitoring their own physiological reactions to the treatment itself to make sure their condition does not deteriorate. By doing so, modelling may be able to provide an early warning system that the treatment is having a negative impact, thereby affording caregivers sufficient time to take appropriate action.
Specifically, this approach combines two different types of information to create its early warning system model. This first is static data, or that which was collected prior to the treatment plan beginning. This includes things like the patient’s demographics, their medical history and how they may have reacted to prior treatments. The second is time-series data, which is information collected in real-time during the course of the treatment. This includes such factors as the specific medication being administered, the results of various tests, their body temperature, hydration levels and blood pressure.
This type of cancer modelling is very much a developing technique and has only been used in small-scale trials thus far. The idea, however, is that by analysing the two datasets in conjunction, the computer can anticipate when a patient is reacting badly to a treatment plan and sound an alarm. While there is the risk that the system might be too sensitive and deliver too many false positives, thus leading to alarm fatigue among the medical staff, the technique has showed encouraging results in early studies.
What about Covid-19 and cancer modelling?
One other way in which cancer modelling has been used to help researchers and medical teams is its application during the pandemic. According to the NHS, lockdown restrictions meant that fewer people were reporting symptoms to their GP, thus leading to a 70% drop in cancer referrals and tests in one local network during the early stages of the pandemic.
This drop-off was noticeable by comparing referral and testing rates with those prior to the onset of the coronavirus pandemic. Inevitably, the shortfall will manifest itself in delayed referrals coming at a later date, which is where modelling was able to provide insight. By analysing the vast reams of data available, NHS researchers were able to estimate the number of missed cases and calculate how much capacity for testing might be required in future. As such, cancer modelling is helping the NHS to remain robust even while facing its greatest challenge of the modern era.
Digital Edition
Lab Asia 31.2 April 2024
April 2024
In This Edition Chromatography Articles - Approaches to troubleshooting an SPE method for the analysis of oligonucleotides (pt i) - High-precision liquid flow processes demand full fluidic c...
View all digital editions
Events
Apr 22 2024 Marrakech, Morroco
Making Pharmaceuticals Exhibition & Conference
Apr 23 2024 Coventry, UK
Apr 23 2024 Kintex, South Korea
Apr 23 2024 Seoul, South Korea
Apr 24 2024 Jakarta, Indonesia


.jpg)