Abstract
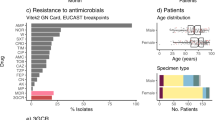
Public health interventions to control the current epidemic of carbapenem-resistant Klebsiella pneumoniae rely on a comprehensive understanding of its emergence and spread over a wide range of geographical scales. We analysed the genome sequences and epidemiological data of >1,700 K. pneumoniae samples isolated from patients in 244 hospitals in 32 countries during the European Survey of Carbapenemase-Producing Enterobacteriaceae. We demonstrate that carbapenemase acquisition is the main cause of carbapenem resistance and that it occurred across diverse phylogenetic backgrounds. However, 477 of 682 (69.9%) carbapenemase-positive isolates are concentrated in four clonal lineages, sequence types 11, 15, 101, 258/512 and their derivatives. Combined analysis of the genetic and geographic distances between isolates with different β-lactam resistance determinants suggests that the propensity of K. pneumoniae to spread in hospital environments correlates with the degree of resistance and that carbapenemase-positive isolates have the highest transmissibility. Indeed, we found that over half of the hospitals that contributed carbapenemase-positive isolates probably experienced within-hospital transmission, and interhospital spread is far more frequent within, rather than between, countries. Finally, we propose a value of 21 for the number of single nucleotide polymorphisms that optimizes the discrimination of hospital clusters and detail the international spread of the successful epidemic lineage, ST258/512.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
All raw and assembled Illumina sequence data are available from the European Nucleotide Archive under the study accession no. PRJEB10018/ERP011196. Individual accession numbers for raw sequence data and de novo assemblies are also available in Supplementary Table 4. Phylogenetic analysis of the 1,717 K. pneumoniae isolates (EuSCAPE only) and the ST258/512 isolates (EuSCAPE and public data) together with all metadata and links to raw sequence data are available at the project URLs https://microreact.org/project/EuSCAPE_Kp and https://microreact.org/project/EuSCAPE_ST258 within Microreact (ref. 51). Phylogenetic analyses and the metadata of the isolates are also available separately for each of the contributing countries in Microreact (see Supplementary Table 7 for project URLs).
References
Global Priority List of Antibiotic-Resistant Bacteria to Guide Research, Discovery, and Development of New Antibiotics (World Health Organization, 2017).
Cassini, A. et al. Attributable deaths and disability-adjusted life-years caused by infections with antibiotic-resistant bacteria in the EU and the European Economic Area in 2015: a population-level modelling analysis. Lancet Infect. Dis. 19, 56–66 (2019).
Mathers, A. J. et al. Molecular dissection of an outbreak of carbapenem-resistant Enterobacteriaceae reveals intergenus KPC carbapenemase transmission through a promiscuous plasmid. mBio 2, e00204-11 (2011).
Martin, J. et al. Covert dissemination of carbapenemase-producing Klebsiella pneumoniae (KPC) in a successfully controlled outbreak: long- and short-read whole-genome sequencing demonstrate multiple genetic modes of transmission. J. Antimicrob. Chemother. 72, 3025–3034 (2017).
Yigit, H. et al. Novel carbapenem-hydrolyzing β-lactamase, KPC-1, from a carbapenem-resistant strain of Klebsiella pneumoniae. Antimicrob. Agents Chemother. 45, 1151–1161 (2001).
Poirel, L., Heritier, C., Tolun, V. & Nordmann, P. Emergence of oxacillinase-mediated resistance to imipenem in Klebsiella pneumoniae. Antimicrob. Agents Chemother. 48, 15–22 (2004).
Yong, D. et al. Characterization of a new metallo-β-lactamase gene, bla NDM-1, and a novel erythromycin esterase gene carried on a unique genetic structure in Klebsiella pneumoniae sequence type 14 from India. Antimicrob. Agents Chemother. 53, 5046–5054 (2009).
Munoz-Price, L. S. et al. Clinical epidemiology of the global expansion of Klebsiella pneumoniae carbapenemases. Lancet Infect. Dis. 13, 785–796 (2013).
Walsh, T. R., Weeks, J., Livermore, D. M. & Toleman, M. A. Dissemination of NDM-1 positive bacteria in the New Delhi environment and its implications for human health: an environmental point prevalence study. Lancet Infect. Dis. 11, 355–362 (2011).
Wang, Y. et al. Comprehensive resistome analysis reveals the prevalence of NDM and MCR-1 in Chinese poultry production. Nat. Microbiol. 2, 16260 (2017).
Albiger, B. et al. Carbapenemase-producing Enterobacteriaceae in Europe: assessment by national experts from 38 countries, May 2015. Eurosurveillance 20, 17–34 (2015).
Kazi, M. et al. Molecular characterization of carbapenem-resistant Enterobacteriaceae at a tertiary care laboratory in Mumbai. Eur. J. Clin. Microbiol. Infect. Dis. 34, 467–472 (2015).
Singh-Moodley, A. & Perovic, O. Antimicrobial susceptibility testing in predicting the presence of carbapenemase genes in Enterobacteriaceae in South Africa. BMC Infect. Dis. 16, 536 (2016).
Grundmann, H. et al. Occurrence of carbapenemase-producing Klebsiella pneumoniae and Escherichia coli in the European Survey of Carbapenemase-Producing Enterobacteriaceae (EuSCAPE): a prospective, multinational study. Lancet Infect. Dis. 17, 153–163 (2017).
Holt, K. E. et al. Genomic analysis of diversity, population structure, virulence, and antimicrobial resistance in Klebsiella pneumoniae, an urgent threat to public health. Proc. Natl Acad. Sci. USA 112, E3574–E3581 (2015).
Long, S. W. et al. Whole-genome sequencing of a human clinical isolate of the novel species Klebsiella quasivariicola sp. nov. Genome Announc. 5, e01057-17 (2017).
Diancourt, L., Passet, V., Verhoef, J., Grimont, P. A. & Brisse, S. Multilocus sequence typing of Klebsiella pneumoniae nosocomial isolates. J. Clin. Microbiol. 43, 4178–4182 (2005).
Aspbury, M. et al. Rapid statistical methods for inferring intra- and inter-hospital transmission of nosocomial pathogens from whole genome sequence data. Preprint at https://www.biorxiv.org/content/10.1101/442319v1 (2018).
Chen, L., Mathema, B., Pitout, J. D. D., DeLeo, F. R. & Kreiswirth, B. N. Epidemic Klebsiella pneumoniae ST258 is a hybrid strain. mBio 5, e01355-14 (2014).
Papp-Wallace, K. M., Endimiani, A., Taracila, M. A. & Bonomo, R. A. Carbapenems: past, present, and future. Antimicrob. Agents Chemother. 55, 4943–4960 (2011).
de Man, T. J. B. et al. Genomic analysis of a pan-resistant isolate of Klebsiella pneumoniae, United States 2016. mBio 9, e00440-18 (2018).
Meletis, G. Carbapenem resistance: overview of the problem and future perspectives. Ther. Adv. Infect. Dis. 3, 15–21 (2016).
Bush, K. et al. Tackling antibiotic resistance. Nat. Rev. Microbiol. 9, 894–896 (2011).
Murray, A. K. et al. Novel insights into selection for antibiotic resistance in complex microbial communities. mBio 9, e00969-18 (2018).
Schwaber, M. J. et al. Containment of a country-wide outbreak of carbapenem-resistant Klebsiella pneumoniae in Israeli hospitals via a nationally implemented intervention. Clin. Infect. Dis. 52, 848–855 (2011).
Falagas, M. E. et al. Risk factors of carbapenem-resistant Klebsiella pneumoniae infections: a matched case-control study. J. Antimicrob. Chemother. 60, 1124–1130 (2007).
Mohan, B. et al. Fecal carriage of carbapenem-resistant Enterobacteriaceae and risk factor analysis in hospitalised patients: a single centre study from India. Indian J. Med. Microbiol. 35, 555–562 (2017).
Bartolini, A. et al. Prevalence, molecular epidemiology and intra-hospital acquisition of Klebsiella pneumoniae strains producing carbapenemases in an Italian teaching hospital from January 2015 to September 2016. Int. J. Infect. Dis. 59, 103–109 (2017).
Yusuf, E. et al. OXA-48 producing Klebsiella pneumoniae in a household contact of a previously infected patient: person-to-person transmission or coincidental community acquisition? Microb. Drug Resist. 22, 134–136 (2016).
Munk, P. et al. Abundance and diversity of the faecal resistome in slaughter pigs and broilers in nine European countries. Nat. Microbiol. 3, 898–908 (2018).
Aanensen, D. M. et al. Whole-genome sequencing for routine pathogen surveillance in public health: a population snapshot of invasive Staphylococcus aureus in Europe. mBio 7, e00444-16 (2016).
Pitart, C. et al. First outbreak of a plasmid-mediated carbapenem-hydrolyzing OXA-48 β-lactamase in Klebsiella pneumoniae in Spain. Antimicrob. Agents Chemother. 55, 4398–4401 (2011).
Snitkin, E. S. et al. Tracking a hospital outbreak of carbapenem-resistant Klebsiella pneumoniae with whole-genome sequencing. Sci. Transl. Med. 4, 148rr116 (2012).
Zhou, K. et al. Use of whole-genome sequencing to trace, control and characterize the regional expansion of extended-spectrum β-lactamase producing ST15 Klebsiella pneumoniae. Sci. Rep. 6, 20840 (2016).
Gu, D. et al. A fatal outbreak of ST11 carbapenem-resistant hypervirulent Klebsiella pneumoniae in a Chinese hospital: a molecular epidemiological study. Lancet Infect. Dis. 18, 37–46 (2018).
Mathers, A. J., Peirano, G. & Pitout, J. D. D. The role of epidemic resistance plasmids and international high-risk clones in the spread of multidrug-resistant Enterobacteriaceae. Clin. Microbiol. Rev. 28, 565–591 (2015).
Cerqueira, G. C. et al. Multi-institute analysis of carbapenem resistance reveals remarkable diversity, unexplained mechanisms, and limited clonal outbreaks. Proc. Natl Acad. Sci. USA 114, 1135–1140 (2017).
Bowers, J. R. et al. Genomic analysis of the emergence and rapid global dissemination of the clonal group 258 Klebsiella pneumoniae pandemic. PLoS ONE 10, e0133727 (2015).
Rodriguez-Zuluet, P. et al. First outbreak of KPC-3-producing Klebsiella pneumoniae (ST258) clinical isolates in a Mexican medical center. Antimicrob. Agents Chemother. 57, 4086–4088 (2013).
Lopez-Cerero, L. et al. Characterisation of the first ongoing outbreak due to KPC-3-producing Klebsiella pneumoniae (ST512) in Spain. Int. J. Antimicrob. Agents 44, 538–540 (2014).
Glasner, C. et al. Carbapenemase-producing Enterobacteriaceae in Europe: a survey among national experts from 39 countries, February 2013. Eurosurveillance 18, 9–15 (2013).
Kock, R. et al. Carbapenem-resistant Enterobacteriaceae in wildlife, food-producing, and companion animals: a systematic review. Clin. Microbiol. Infect. 24, 1241–1250 (2018).
Bolger, A. M., Lohse, M. & Usadel, B. Trimmomatic: a flexible trimmer for Illumina sequence data. Bioinformatics 30, 2114–2120 (2014).
Bankevich, A. et al. SPAdes: a new genome assembly algorithm and its applications to single-cell sequencing. J. Comput. Biol. 19, 455–477 (2012).
Gurevich, A., Saveliev, V., Vyahhi, N. & Tesler, G. QUAST: quality assessment tool for genome assemblies. Bioinformatics 29, 1072–1075 (2013).
Ondov, B. D. et al. Mash: fast genome and metagenome distance estimation using MinHash. Genome Biol. 17, 132 (2016).
Li, H. & Durbin, R. Fast and accurate short read alignment with Burrows−Wheeler transform. Bioinformatics 25, 1754–1760 (2009).
Seemann, T. Prokka: rapid prokaryotic genome annotation. Bioinformatics 30, 2068–2069 (2014).
Page, A. J. et al. Roary: rapid large-scale prokaryote pan genome analysis. Bioinformatics 31, 3691–3693 (2015).
Stamatakis, A. RAxML-VI-HPC: maximum likelihood-based phylogenetic analyses with thousands of taxa and mixed models. Bioinformatics 22, 2688–2690 (2006).
Argimón, S. et al. Microreact: visualizing and sharing data for genomic epidemiology and phylogeography. Microb. Genom. 2, e000093 (2016).
Hunt, M. et al. ARIBA: rapid antimicrobial resistance genotyping directly from sequencing reads. Microb. Genom. 3, e000131 (2017).
Wyres, K. L. et al. Identification of Klebsiella capsule synthesis loci from whole genome data. Microb. Genom. 2, e000102 (2016).
Altschul, S. F., Gish, W., Miller, W., Myers, E. W. & Lipman, D. J. Basic local alignment search tool. J. Mol. Biol. 215, 403–410 (1990).
Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria That Grow Aerobically 10th edn (CLSI, 2015).
Deleo, F. R. et al. Molecular dissection of the evolution of carbapenem-resistant multilocus sequence type 258 Klebsiella pneumoniae. Proc. Natl Acad. Sci. USA 111, 4988–4993 (2014).
Croucher, N. J. et al. Rapid phylogenetic analysis of large samples of recombinant bacterial whole genome sequences using Gubbins. Nucleic Acids Res. 43, e15 (2015).
Hadfield, J. et al. Phandango: an interactive viewer for bacterial population genomics. Bioinformatics 34, 292–293 (2018).
Acknowledgements
We thank the Pathogen Informatics Group and Core Sequencing Facility at the Wellcome Sanger Institute for their contributions to the study. We also thank F. Bosma and M. Zigterman from the Medical Microbiology and Infection Prevention Department of the University Medical Center Groningen for their support in assembling the isolate collection. This work was funded by The Centre for Genomic Pathogen Surveillance, Wellcome Genome Campus, Wellcome (grant nos. 098051 and 099202) and the NIHR Global Health Research Unit on Genomic Surveillance of Antimicrobial Resistance (NIHR 16/136/111). The EuSCAPE project was funded by ECDC through a specific framework contract (ECDC/2012/055) following an open call for tender (OJ/25/04/2012-PROC/2012/036). This work was carried out on behalf of the ESCMID Study Group for Epidemiological Markers (ESGEM); the full list of members is provided in the Supplementary Information.
Author information
Authors and Affiliations
Consortia
Contributions
H.G. and D.M.A. conceived the study. The EuSCAPE Working Group collected the bacterial isolates and epidemiological data and performed preliminary laboratory analyses. The ESGEM facilitated the training and capacity building for the collection of bacterial isolates and preliminary analyses. S.D., S.R., S.R.H., C.G., T.F., S.A., K.A., R.G., T.G., G.E., M.A., S.S., E.J.F., G.M.R., H.G. and D.M.A. performed the data analysis. S.D., S.R., E.J.F., G.M.R., H.G. and D.M.A. wrote the manuscript. All authors read and approved the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary Figs. 1–3, Supplementary Table 1, Supplementary Table 5, Supplementary Table 7 and Supplementary Note.
Supplementary Table 2
Detailed QC results for all sequenced isolates submitted as K. pneumoniae.
Supplementary Table 3
Identification of best-matching taxa to the individual assembly contigs of all sequenced isolates using Mash.
Supplementary Table 4
Epidemiological and genotyping data for 1,717 K. pneumoniae isolates that passed sequencing QC filters.
Supplementary Table 6
Epidemiological and genotyping data and publication sources of 651 isolates used in the ST258/512 phylogenetic analysis.
Rights and permissions
About this article
Cite this article
David, S., Reuter, S., Harris, S.R. et al. Epidemic of carbapenem-resistant Klebsiella pneumoniae in Europe is driven by nosocomial spread. Nat Microbiol 4, 1919–1929 (2019). https://doi.org/10.1038/s41564-019-0492-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41564-019-0492-8
This article is cited by
-
Genomic surveillance for antimicrobial resistance — a One Health perspective
Nature Reviews Genetics (2024)
-
Capsules and their traits shape phage susceptibility and plasmid conjugation efficiency
Nature Communications (2024)
-
Global epistasis in plasmid-mediated antimicrobial resistance
Molecular Systems Biology (2024)
-
Elimination of blaKPC−2-mediated carbapenem resistance in Escherichia coli by CRISPR-Cas9 system
BMC Microbiology (2023)
-
In-vitro antibacterial activity and mechanism of Monarda didyma essential oils against Carbapenem-resistant Klebsiella pneumoniae
BMC Microbiology (2023)